CELL:临床试验表明,剖宫产婴儿接受母亲粪便移植可恢复肠道微生物发育
2020-10-03 haibei MedSci原创
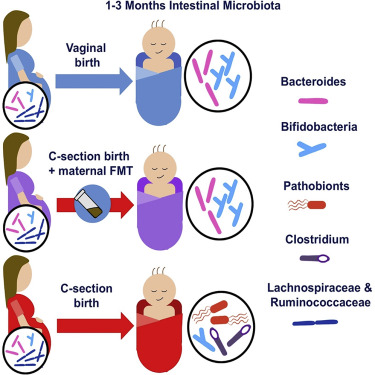
新生儿的微生物定植是影响日后健康的关键过程。深度元基因组学分析和近期的菌株水平剖析显示,正常婴儿肠道中的早期优势菌是母体粪便细菌,主要是双歧杆菌和双歧杆菌的成员。停止母乳喂养后,粪便微生物群逐渐变得以
新生儿的微生物定植是影响日后健康的关键过程。深度元基因组学分析和近期的菌株水平剖析显示,正常婴儿肠道中的早期优势菌是母体粪便细菌,主要是双歧杆菌和双歧杆菌的成员。停止母乳喂养后,粪便微生物群逐渐变得以厌氧梭菌为主。这种一般模式在不同人群中都很明显,很可能代表了人类正常发育不可或缺的生物决定性现象。因此,人类系统很可能已经适应了在某些时间窗口接收特定的微生物信号,以便在早期生命中进行相互的免疫和代谢编程。
自然微生物群的定植和发育可能会被阻止母体传播细菌或改变婴儿体内微生物群的做法所扰乱。剖腹产(CS)分娩是破坏正常菌落过程的最强因素之一。这种做法有效地消除了出生时肠道细菌从母亲到婴儿的自然垂直转移的可能性,导致微生物群发展的偏差,且最明显的是在生命的前6个月。
CS分娩在全球范围内越来越多,在某些地区影响了超过50%的婴儿,并且有新的证据表明,通过CS出生的婴儿有不同的细菌和其他暴露,可能会微妙地改变新生儿生理学。
一些研究表明,CS出生与短期和长期影响相关,包括慢性免疫疾病风险的增加。然而,关于CS分娩的影响仍存在争议,应该注意的是,早产、使用抗生素和其他混杂因素可能会影响所报道的关联。一些大型研究发现,CS分娩与特定疾病,如1型糖尿病,无关。
相比之下,最近丹麦的一项研究包含了1982-2010年间超过250万的分娩案例,并进行了长达40年的随访。结果显示,与阴道分娩的孩子相比,CS出生的孩子患四种常见的、由免疫介导的医院诊断的儿童慢性炎症疾病的风险增加,包括炎症性肠病、类风湿性关节炎、乳糜泻和1型糖尿病。值得注意的是,最近一项基于英国的大型队列研究显示,CS出生的婴儿微生物群发育迟缓,病原体水平增加,母婴微生物群转移受损。
除了对个体的影响外,这种普遍缺乏垂直细菌转移的现象可能会产生代际效应,当母女之间的肠道细菌遗传被消除后,某些与宿主共同适应了几千年的互生菌是否有可能永久消失。
越来越多的证据表明,肠道微生物群对儿童整体发育的重要性,这就提出了尽早纠正CS分娩造成的微生物群失衡的需求。由于婴儿肠道在出生时通常由母体肠道微生物定植,因此,为CS出生婴儿的微生物群播种的最天然接种物是母体粪便。
最近,研究人员在CELL杂志发文,其进行了一项临床试验(在临床试验中注册为NCT03568734),探讨了母亲对自己婴儿的粪便微生物群移植(FMT)是否安全有效地恢复CS出生婴儿早期的正常肠道微生物群及其发育。
在该研究中,总共有17名即将以剖腹产方式分娩的孕妇参加了产后胎儿粪便移植的研究。其中7位经过仔细筛选后被选中。她们的婴儿接受了来自自己母亲分娩前3周的稀释粪便样本。
在3个月的随访中,7名婴儿的临床过程都很顺利,没有出现不良反应。FMT治疗的CS出生婴儿的粪便微生物群组成的时间发展不再与未经治疗的CS出生婴儿相似,但与阴道出生婴儿的粪便微生物群组成表现出显著的相似性。
这项概念验证研究表明,CS出生婴儿的肠道微生物群可以通过母体FMT在产后恢复。但是,这必须在经过仔细的临床和微生物学检查后才能进行。
原始出处:
Katri Korpela et al. Maternal Fecal Microbiota Transplantation in Cesarean-Born Infants Rapidly Restores Normal Gut Microbial Development: A Proof-of-Concept Study. CELL (2020). DOI: https://doi.org/10.1016/j.cell.2020.08.047
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
35
#微生物#
41
#CEL#
42
#发育#
48
#粪便#
0