EBCAM:罗哌卡因和利多卡因在双眼皮整形术中有何不同?
2022-06-30 医路坦克 MedSci原创
双眼皮整形术是一种改变眼皮结构,重塑眼皮,形成新的上眼皮褶皱的手术。本研究旨在比较评估罗哌卡因和利多卡因在双眼皮重睑术中的效果。
双眼皮整形术是一种改变眼皮结构,重塑眼皮,形成新的上眼皮褶皱的手术。在美学上,双眼皮比单眼皮更有立体感,因为它的眼裂宽而长,层次丰富,角膜暴露的部分更多。在中国,有40%的人是单眼皮,这极大地刺激了对双眼皮整形术的需求。
目前,重睑术主要有埋线法和切开法,通过埋线法将睑板腺-提肌腱膜与皮下眼轮匝肌缝合,形成临时性的缝合固定。然而,眼睑的组织细胞会对埋藏的缝线产生炎症反应,并产生自体胶原纤维来包裹缝线,形成对自体组织的替代。更糟糕的是,缝线会松动,随后,新形成的胶原纤维会取代埋藏的缝线。
切开法是沿着设计的切口线水平切开皮肤,重新调整眶隔脂肪的体积,减薄眼轮匝肌,并调整提肛肌腱膜和跗骨板的结合状态,形成皮肤-眼轮匝肌和眼睑-提肛肌腱膜之间的直接连接。
由于切开法具有效果持久、适应症广泛等优点,已被广泛认可。然而,双眼皮整形术对术中局部浸润麻醉和术后镇痛的要求很高。优秀的麻醉和镇痛可以减少疼痛引起的紧张、焦虑和恐惧,有助于获得良好的手术效果和满意度。
利多卡因是双眼皮切口麻醉的常用药物,而它存在作用时间短、皮肤肿胀等缺点。罗哌卡因是一种L-体长效酰胺类局麻药。它可以通过阻断钠离子流入神经纤维的细胞膜而可逆地阻断神经纤维的冲动传导;此外,它还具有麻醉和镇痛的双重作用,因此在手术区阻断和硬膜外麻醉以及术后硬膜外麻醉中普遍使用。如前所述,利多卡因是一种中效局麻药,罗哌卡因是一种长效局麻药。两者都用于外科手术,而它们的差异至今尚未被研究。
为了弥补这一空白,我们打算比较这两种麻醉方法的疗效。
这项前瞻性随机对照研究旨在比较评估罗哌卡因和利多卡因在双眼皮重睑术中的效果。从2019年1月至2021年7月在我院美容科接受双眼皮整形术的患者共120人,随机(1 :1)分为对照组(1%利多卡因-肾上腺素混合物)和研究组(0.75%罗哌卡因-肾上腺素混合物导致术后2小时至1天的Wong-Baker FACES疼痛评级视觉模拟量表得分低于1%利多卡因-肾上腺素混合物(所有P < 0.05)。两组的手术时间、术中麻醉药物用量和术中失血量相似(所有P<0.05)。 0.75%罗哌卡因-肾上腺素混合液的术后肿胀评分较低,但与1%利多卡因-肾上腺素混合液相比,患者满意度评分较高(所有P<0.05)。
表1:两组患者一般情况比较
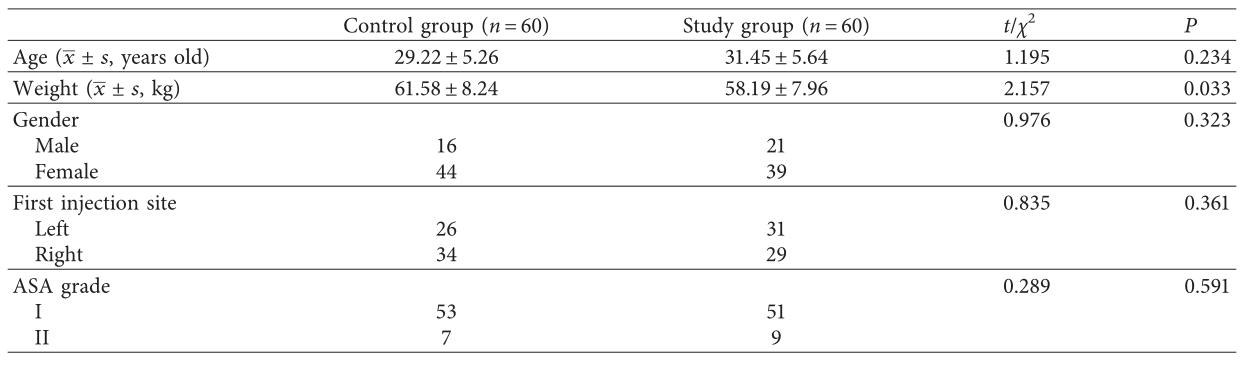
图2:两组患者术后疼痛情况比较。∗∗P < 0.01。∗∗∗P < 0.001
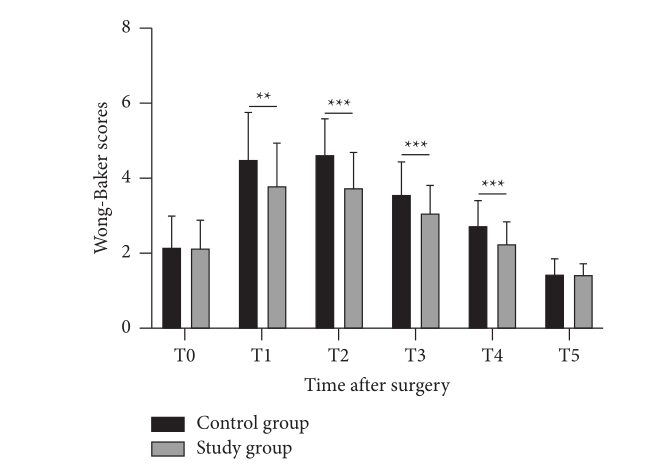
图3:两组患者出血量评分(a)、肿胀评分(b)比较。∗∗∗P < 0.001。
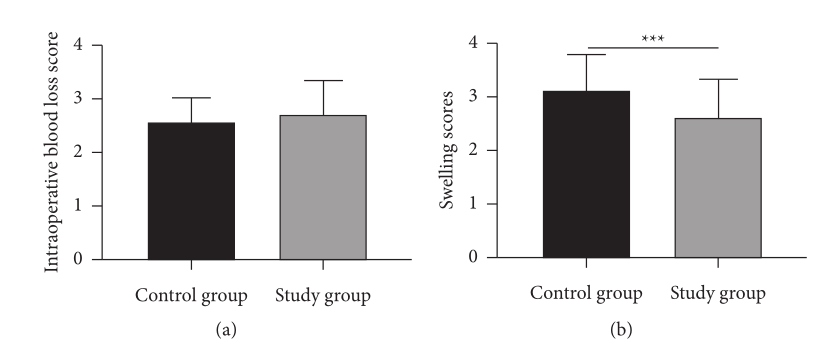
结果发现两组的安全状况相似(所有P < 0.05)。利多卡因和罗哌卡因在双眼皮整形术中都能产生理想的麻醉效果。罗哌卡因可以明显减少术后疼痛,减轻术后肿胀,满意度更高,因此值得进一步推广。
文献来源: Liu S, Chu Z,Ropivacaine and Lidocaine in Double Eyelid Blepharoplasty: A Comparative Analysis.Evid Based Complement Alternat Med 2022;2022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CAM#
44
#整形术#
48
#利多卡因#
41
#罗哌卡因#
40