Cell Death Dis:他汀类药物在p53突变型T型淋巴瘤中的抗癌作用
2020-05-10 QQY MedSci原创
长期以来的研究发现他汀类药物可能具有抗肿瘤活性。目前一些流行病学的证据显示,他汀类药物的使用与许多散发性癌症(包括大肠癌、乳腺癌、肺癌、前列腺癌和肾癌)的死亡率降低息息相关。
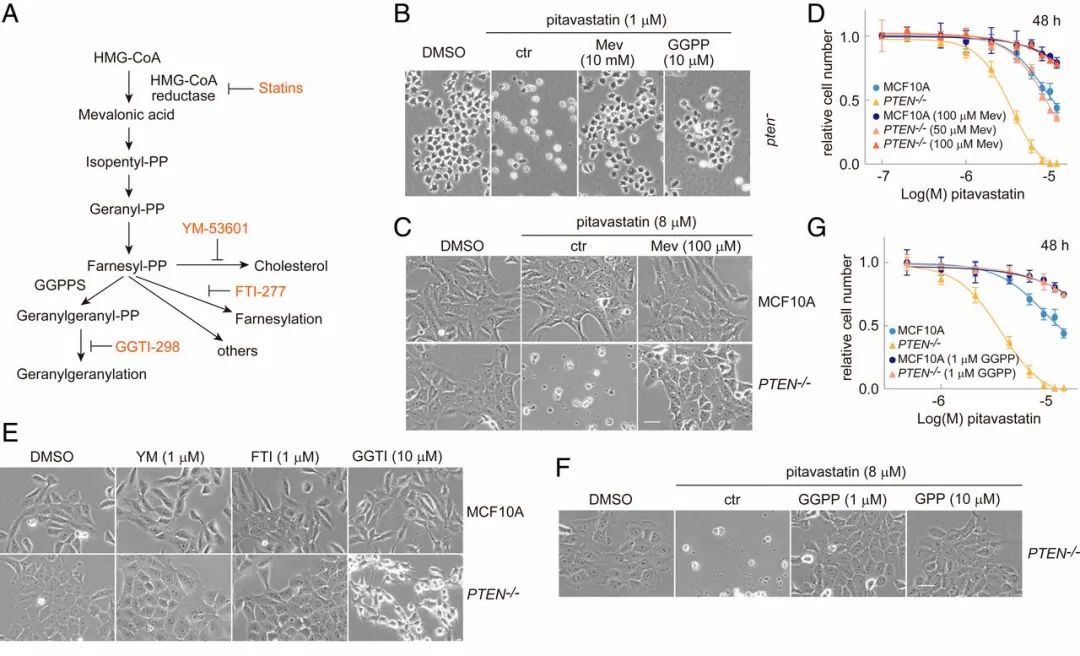
基于细胞和动物模型的临床研究发现,他汀类药物能够直接抑制前列腺癌和胰腺癌的发生发展。TP53是人类癌症中最常见的突变基因。大多数p53突变为错义突变(mutp53),这种突变不仅失去了p53的抑癌功能,而且还经常会有促癌的获得功能(GOF),促进癌症的发生发展、EMT、侵袭、代谢、转移和化学耐药性。 Mutp53蛋白的稳定是GOF的先决条件。mutp53的GOF作用主要表现在稳定的mutp53蛋白能够增强甲羟戊酸途径,而该机制也为探索他汀类药物中的HMGCoA还原酶抑制剂作为mutp53肿瘤的抗癌药提供了理论基础。
在该研究中,研究人员揭示了他汀类药物在表达两种不同GOF mutp53等位基因的晚期临床T细胞淋巴瘤小鼠模型中的治疗效果。
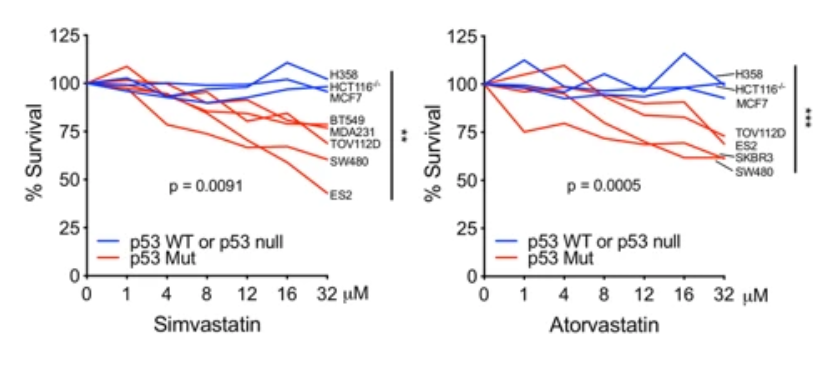
用瑞舒伐他汀单药治疗的表达p53 R248Q突变体的T淋巴瘤可获得一定程度的p53等位基因选择性和短暂的抗肿瘤作用,而在表达p53 R172H突变体的肿瘤中则没有这些现象;此外,缺乏p53的小鼠也没有这些作用。他汀类药物的体外敏感性并不能作为其体内敏感性的预测指标,皮下移植瘤的实验结果则可以作为预测指标。
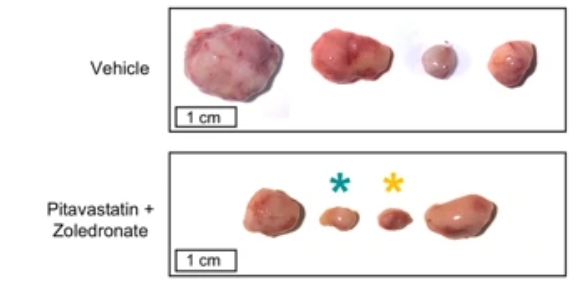
本研究表明,在联合疗法中加入他汀类药物或可改善抗肿瘤作用,同时确定了在稳定p53突变体癌症中对他汀类药物最敏感的等位基因和肿瘤类型。
原始出处:
Tutuska et al. Statin as anti-cancer therapy in autochthonous Tlymphomas expressing stabilized gain-of-function mutant p53 proteins. Cell Death and Disease (2020) 11:274
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
0
#CEL#
40
#突变型#
46
#Cell#
45
#他汀类药#
39
#p53#
30
#Death#
47