Lancet:肺段切除术有望成为小外周NSCLC的标准术式!
2022-04-26 Nebula MedSci原创
肺段切除术可成为小外周 NSCLC 患者的标准手术方式
肺癌是全球癌症相关死亡的主要原因,而且发病率持续增加。肺叶切除术是早期非小细胞肺癌 (NSCLC) 的标准疗法。但随着筛查技术的进步,越来越多患者在极早期获得诊断,因此,亚肺叶切除的实际适应症已扩展到早期肺癌。但目前尚未在随机试验环境中评估肺段切除术的生存率和临床益处。
本研究旨在调查在小周围 NSCLC 患者中,肺段切除术是否不劣于肺叶切除术。
这是一项随机对照、非劣效性临床试验,招募了临床IA期的NSCHC患者(肿瘤直径≤2 cm,实变肿瘤比>0.5),随机(1:1)分成两组,接受肺叶切除术或肺段切除术。主要终点是总生存率;次要终点包括术后肺功能(6个月和12个月)、无复发生存率、局部复发率、不良反应、肺段切除完成比例、住院时长、胸管放置时长、手术时长、出血量和外科自动缝合钉的使用数量。
2009年10月10日-2014年10月21日期间,共招募了1106位患者:肺叶切除术组 554位,肺段切除术组 552位。基线时两组患者的临床病理因素均衡。在肺段切除术组,有22位患者转为肺叶切除术,,还有一位患者接受了宽楔形切除术。
两组的5年总生存率
中位随访了7.3年,肺段切除术组和肺叶切除术组的5年总生存率分别是94.3%和91.1%,通过分层Cox回归模型确认了总生存期的优效性和非劣效性(HR 0.663,非劣效性 p<0.001,优越性 p=0.0082)。在所有预定义亚组中均观察到了肺段切除术的总生存预后益处。
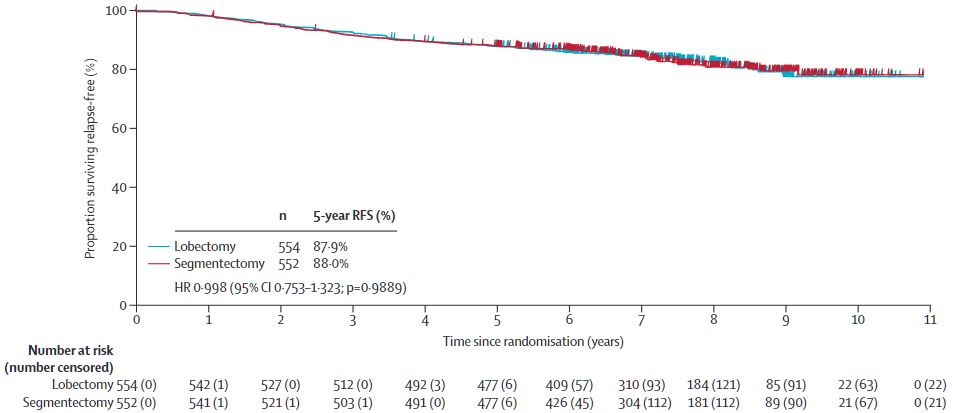
两组的5年无进展生存率
在第1年随访期间,两组的1秒用力呼气中位减少量差异显著(3.5%,p<0.0001),但未达到预定义的临床意义阈值10%。肺段切除术组和肺叶切除术组的5年无复发生存率分是88.0%和87.9%(HR 0.998, p=0.9889)。肺段切除术组和肺叶切除术组的局部复发率分别是10.5%和5.4%(p=0.0018)。
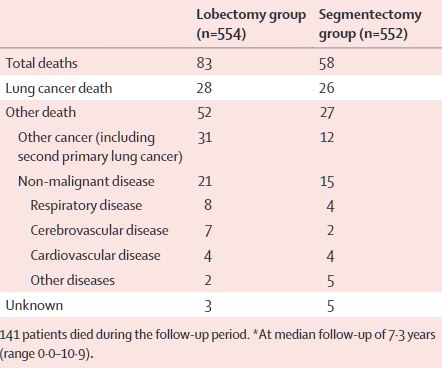
两组随访期间的死亡病例
肺叶切除术后和肺段切除术后分别有52位(63%,总83位)和27位(47%,58位)死于其他疾病。术后90天内无死亡病例。两组术后2级及以上的并发症的发生率相近(肺叶切除术组 vs 肺段切除术组:26% vs 27%)。
据了解,这项研究是首个证明肺段切除术与肺叶切除术对小外周 NSCLC 患者总生存期益处的 3 期试验。研究结果表明,肺段切除术可成为这类患者的标准手术方式。
原始出处:
Hisashi Saji, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. The Lancet. April 23, 2022. https://doi.org/10.1016/S0140-6736(21)02333-3.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肺段切除术#
51
#切除术#
40
#Lancet#
42
***。
60
lancet上果然牛,感谢梅斯更新及时
35