ASCO2022:TROPiCS-02临床重磅发布:戈沙妥珠单抗使HR+/HER2-MBC进展或死亡降低34%!
2022-06-11 MedSci原创 MedSci原创
戈沙妥珠单抗(sacituzumab govitecan)对比医生选择的治疗方案用于激素受体阳性/HER2阴性晚期乳腺癌患者的疗效——随机III期TROPiCS-02研究
HR+/HER2-是最常见的转移性乳腺癌(MBC)亚型。治疗包括序贯内分泌治疗联合靶向药物,然后是单药化疗,受益持续时间越来越短。戈沙妥珠单抗(sacituzumab govitecan,SG)是一种抗trop-2抗体药物偶联物,被批准用于既往治疗≥2次的转移性三阴性乳腺癌(MBC≥1次)。在1/2期imu-132-01研究中,HR+/HER2- MBC队列(n = 54)的客观缓解率(ORR)为31.5%,中位无进展生存期(PFS)为5.5个月,中位总生存期(OS)为12个月,SG的安全性可控。TROPiCS-02是一项3期随机研究(NCT03901339),旨在证实SG在HR+/HER2-晚期乳腺癌中的效果。
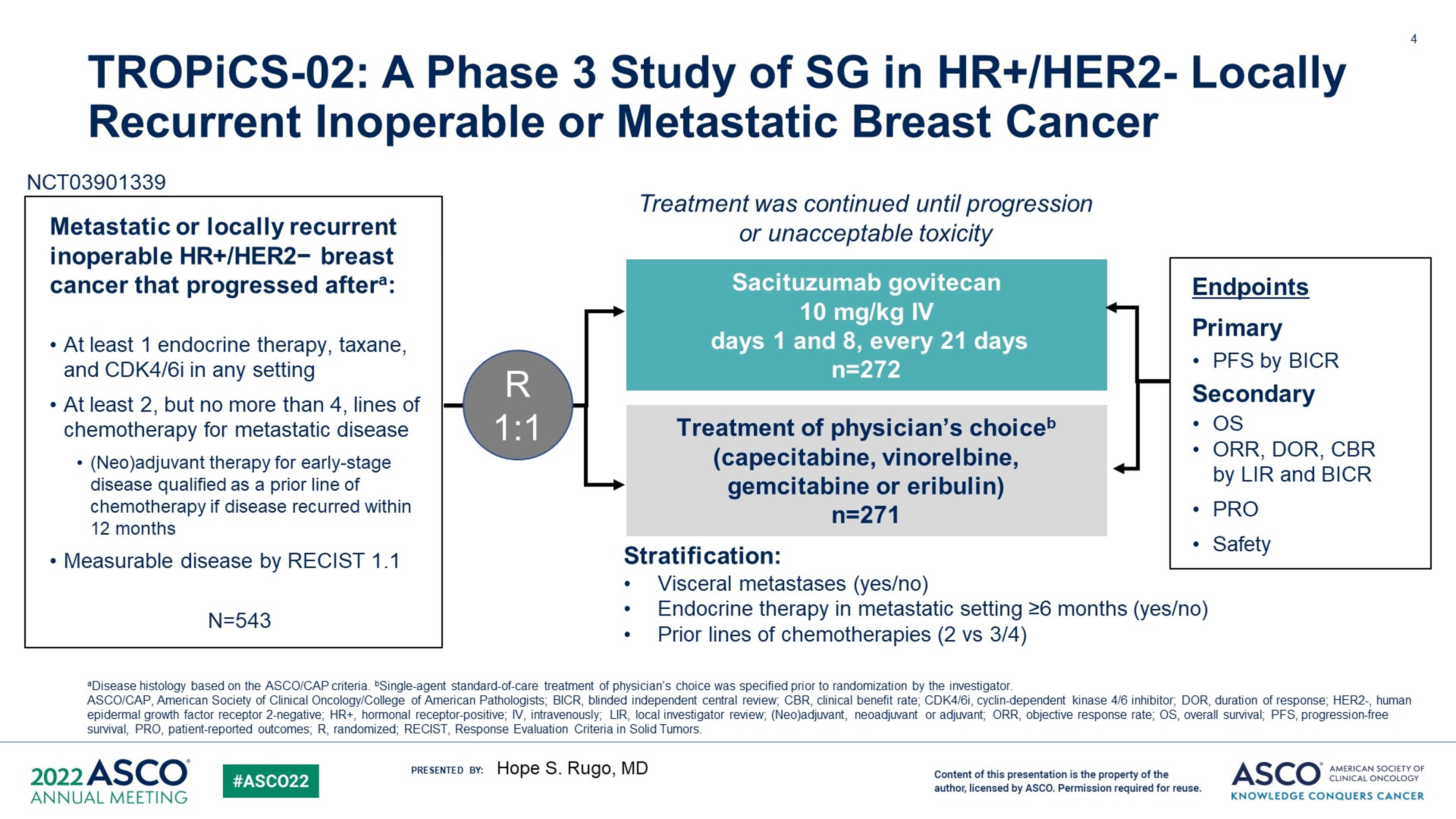
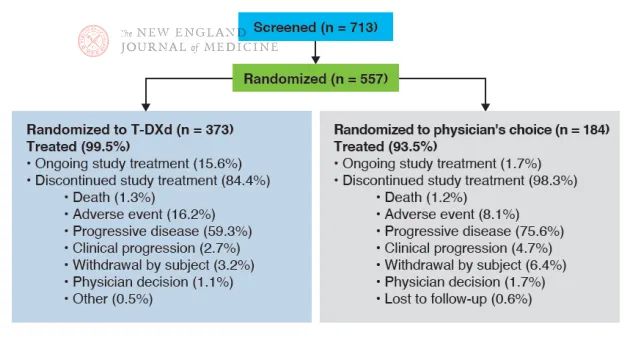
本研究纳入了局部确定的HR+/HER2-不可切除的局部晚期或MBC, ECOG体力状态评分为0或1,以及既往化疗方案为2-4次的MBC成年人。如果在(新)辅助治疗后疾病进展≤12个月,允许既往1次MBC治疗。在任何情况下,患者必须接受过≥1次紫杉烷、CDK4/6抑制剂和内分泌治疗。将患者按1:1随机分组,接受SG(每21天为一周期,第1天和第8天10 mg/kg 静脉注射)或TPC(卡培他滨、艾力布林、长春瑞滨或吉西他滨),直到疾病进展/出现不可接受的毒性。主要终点为根据RECIST v1.1进行的独立盲法中心评价(最终分析)的PFS,关键次要终点为OS(第1个计划的中期分析)。
在2022年1月3日数据截止时,分别有272名和271名患者被随机分配到SG组和TPC组。SG组和TPC组的Pt特征相似(MBC 3个中位既往化疗方案[范围,0-8];95%有内脏转移,86%的MBC≥6个月之前接受过内分泌治疗,分别有60%和38%的MBC在≤12个月和> 12个月之前接受过CDK4/6抑制剂)。
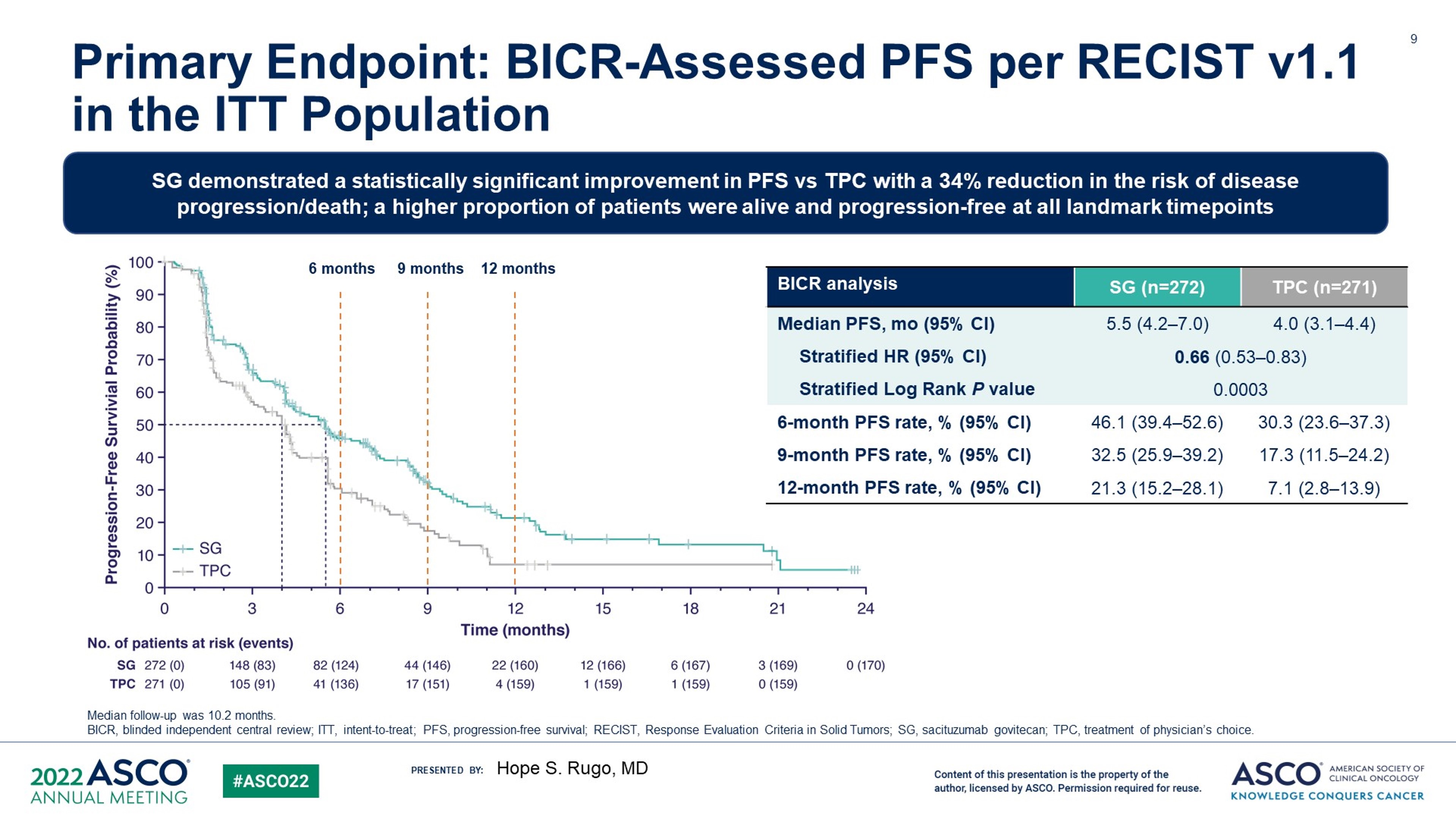
相比起TPC,SG显著改善了中位PFS (5.5 vs 4.0个月;HR,0.66;95%CI,0.53-0.83;P = 0.0003); SG和TPC的6个月和12个月PFS率分别为46% vs 30%和21% vs 7%。
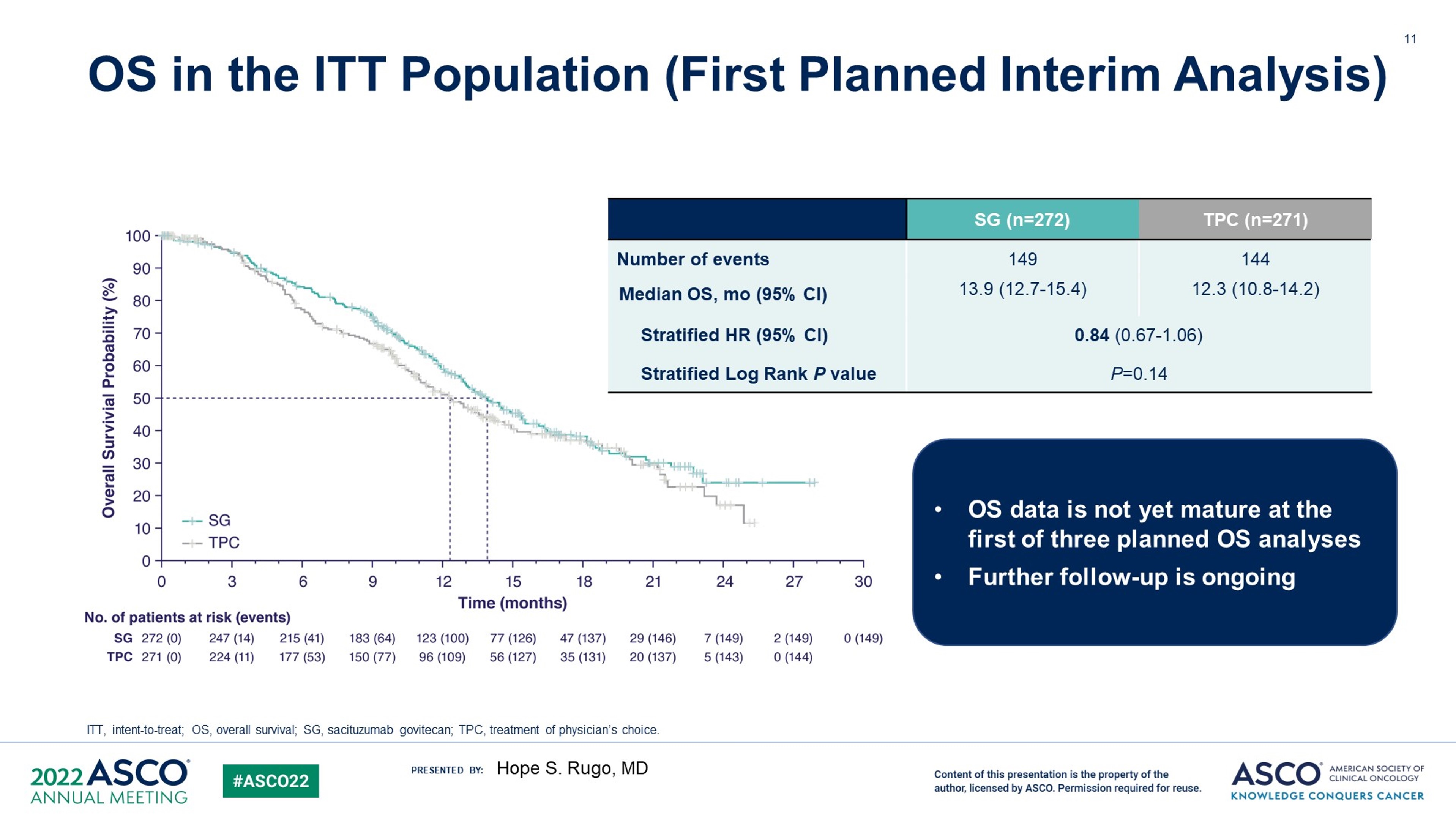
SG相较TPC在OS上显示出数值性的优势,但无统计学意义 (13.9 vs 12.3个月;HR,0.84;P = 0.143);SG组的ORR (21% vs 14%)和临床获益率(34% vs 22%)均高于TPC组,中位缓解持续时间分别为7.4个月vs 5.6个月。
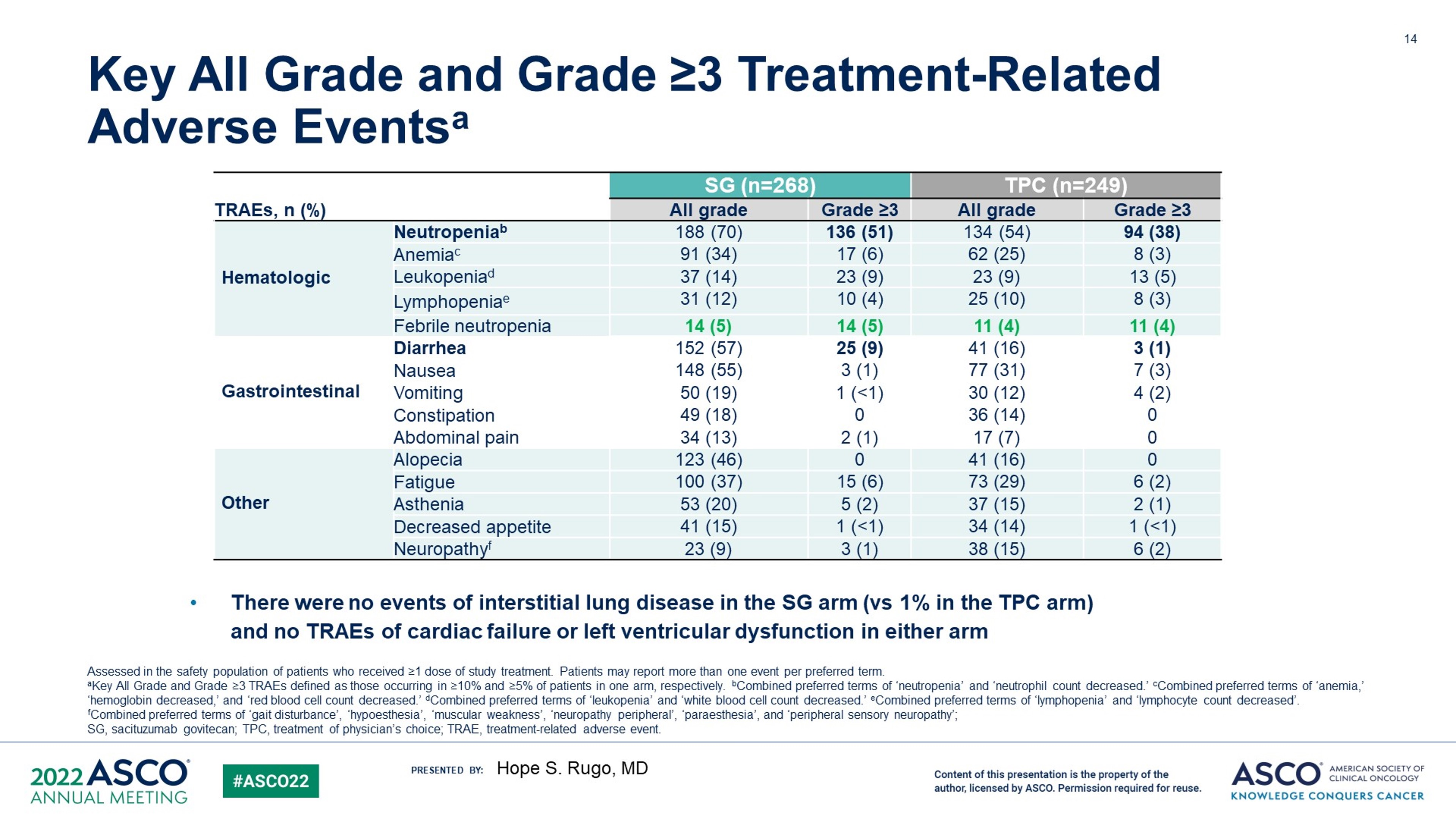
总体而言,在SG组和TPC组中分别有 74%和60%患者发生≥3级的治疗相关不良事件(AEs);其中中性粒细胞减少(51% vs 39%)和腹泻(10% vs 1%)最为常见。导致SG停药的AEs比TPC低(6%比4%)。SG组有1例治疗相关死亡;TPC组则没有。
与单药化疗相比,SG表现出显著的PFS获益,对于重度预处理的HR+/HER2内分泌耐药、不可切除的局部晚期或MBC且治疗选择有限的患者,其安全性可控。
原文来源:
https://meetings.asco.org/abstracts-presentations/206927
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ASC#
45
#HER2-#
44
#重磅#
54