ASCO 2022:PALOMA-2研究最终数据出炉:全球首款CDK4/6抑制剂哌柏西利再受挫!
2022-06-11 MedSci原创 MedSci原创
PALOMA-2:哌柏西利联合来曲唑对比安慰剂联合来曲唑一线治疗ER阳性/HER2阴性晚期乳腺癌患者的总生存(OS)。
基于随机II期PALOMA-1研究,哌柏西利(PAL)被批准成为首个用于雌激素受体阳性(ER+)/人表皮生长因子受体2阴性(HER2-) 晚期乳腺癌(ABC)的细胞周期蛋白依赖激酶4/6 (CDK4/6)抑制剂。PALOMA-2是一项随机、双盲、III期临床试验,证实相较安慰剂(PBO)+来曲唑(LET),PAL+LET一线治疗ER+/HER2- ABC能显著改善无进展生存期(PFS) (中位PFS,27.6个月vs 14.5个月;HR,0.56 [95% CI, 0.46-0.69]; P<0.0001)。在最终PFS分析时,OS数据还不成熟。此次分析报告了OS结果。
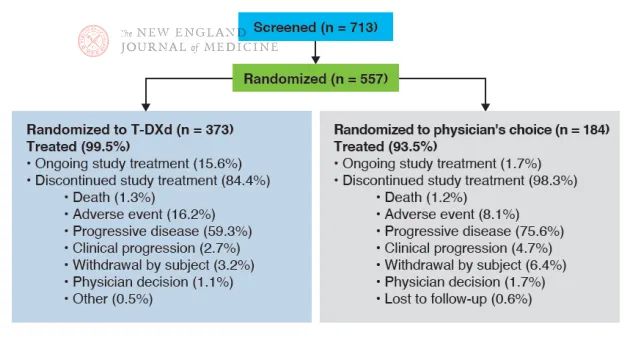
666名既往未接受过晚期全身治疗的绝经后ER+/HER2- ABC女性,按2:1比例被随机分配到PAL (125mg/d口服,3/1周计划)+LET (2.5 mg/d口服,连续)组或PBO+LET组。主要终点是研究者评估的PFS,关键次要终点是OS。在每项研究设计中,390个OS事件需要有80%效能才能使用分层对数秩检验在显著性水平0.025(单侧)下检测到HR<0.74。当观察到分析所需的事件数量时,进行计划的最终OS分析。

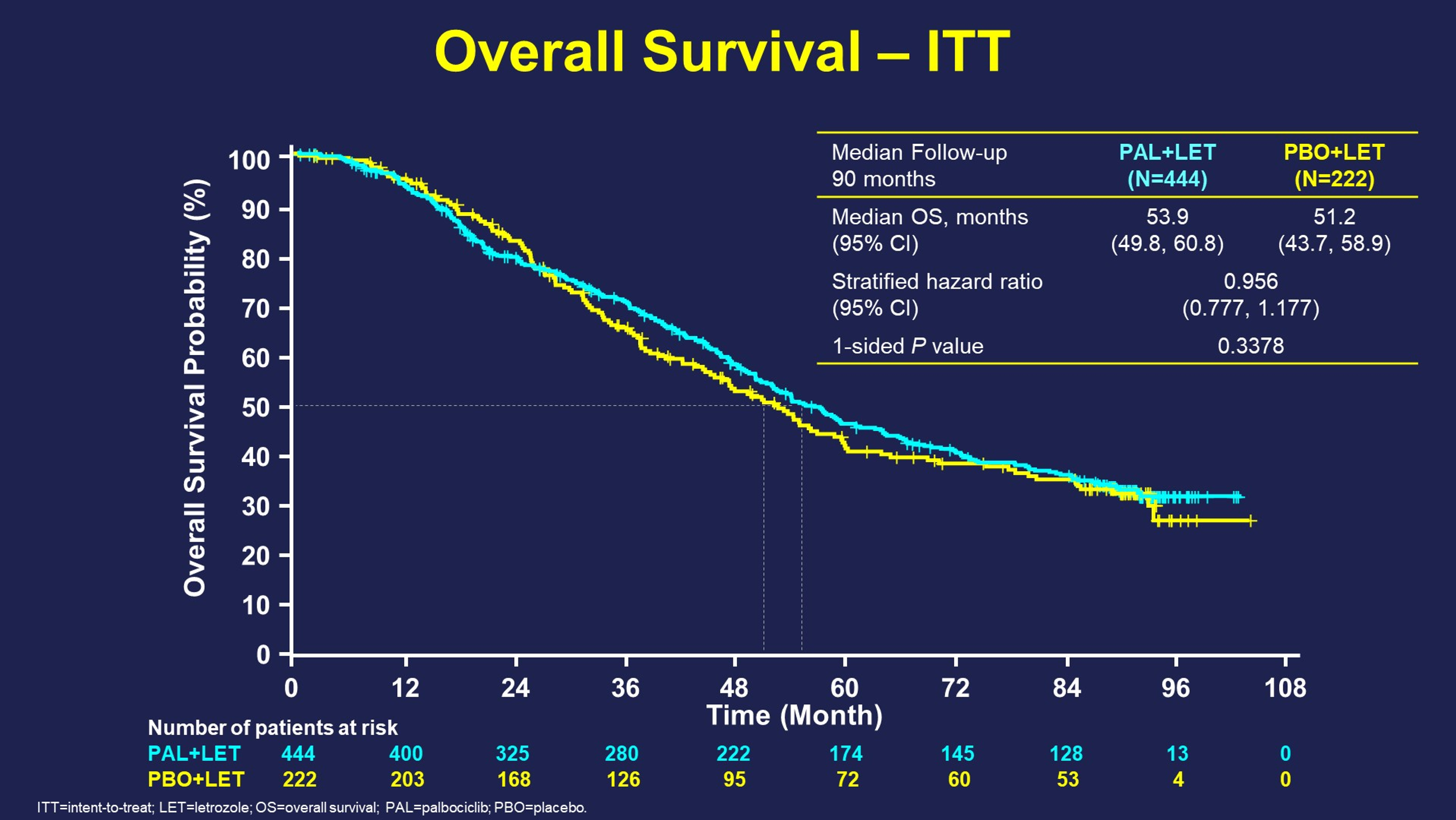
数据截止时(2021年11月15日),中位随访时间为90个月,分别共有43例 (10%) 和5例(2%)仍在PAL+LET组和PBO+LET组。405例死亡中,两组的中位OS(95% CI)分别为53.9个月(49.8-60.8)和为51.2个月 (43.7-58.9) (HR,0.956 ;95% CI, 0.777-1.177;分层单侧P = 0.3378)。
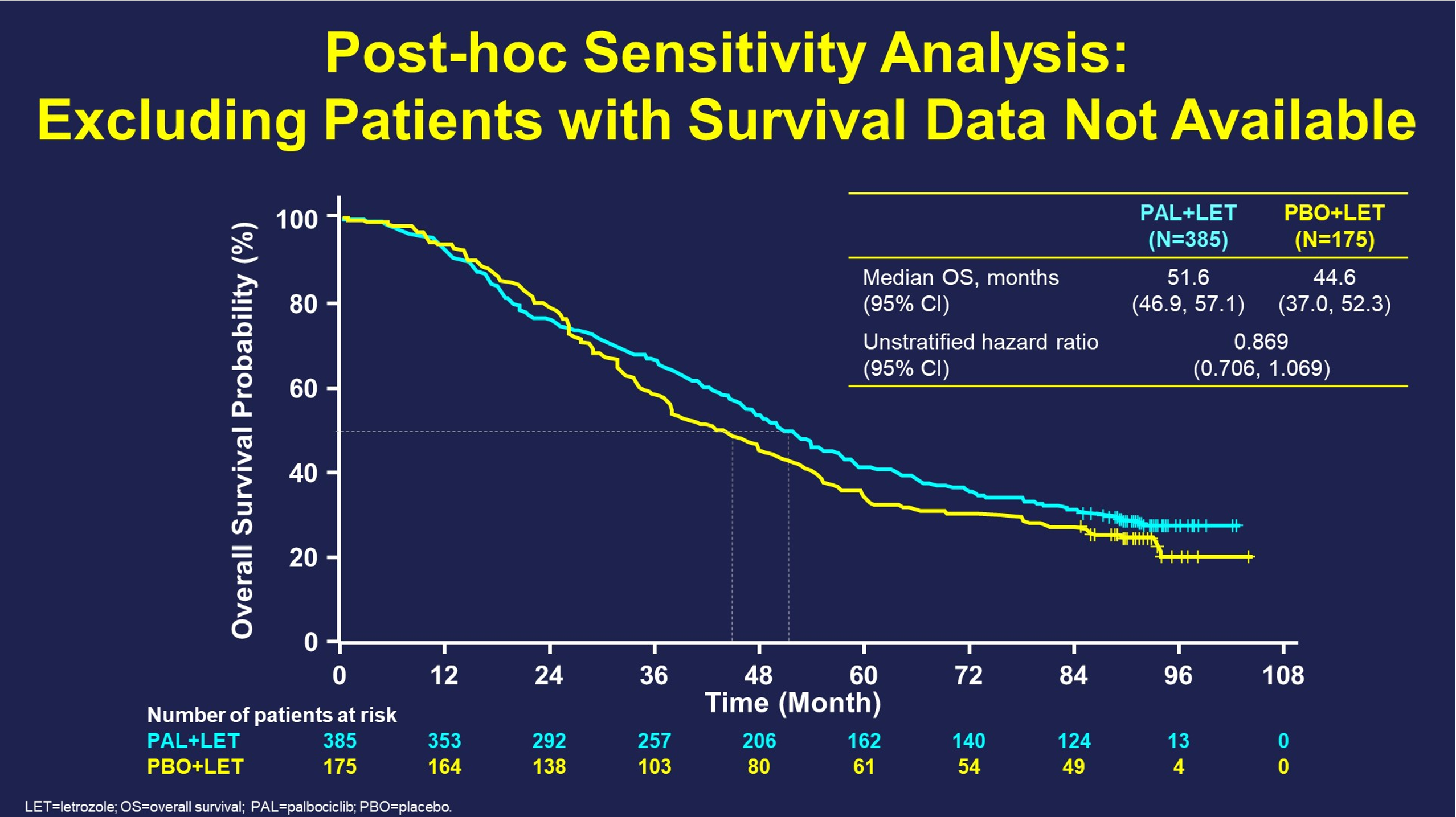
在这一OS分析中,PBO+LET组的21%以及PAL+LET组的13%患者无法进行随访(撤回同意或失去随访)并接受审查。排除这些患者后的敏感度分析显示,PAL+LET组的中位OS (95% CI)为51.6个月(46.9-57.1),PBO+LET组的中位OS (95% CI)为44.6个月(37.0-52.3)(HR,0.869 ;95% CI, 0.706-1.069)。
在停止研究治疗的患者中,81%的PAL+LET组和88%的PBO+LET组患者接受了研究后全身治疗;停用患者中分别有12%和27%接受了CDK4/6抑制剂治疗。在无病间隔(DFI) >12个月的患者中,PAL+LET组和PBO+LET组的中位OS (95% CI)分别为66.3 (52.1-79.7)(n=179)和47.4个月 (37.7-57.0) (n=93);(HR,0.728 ;95% CI, 0.528-1.005)。

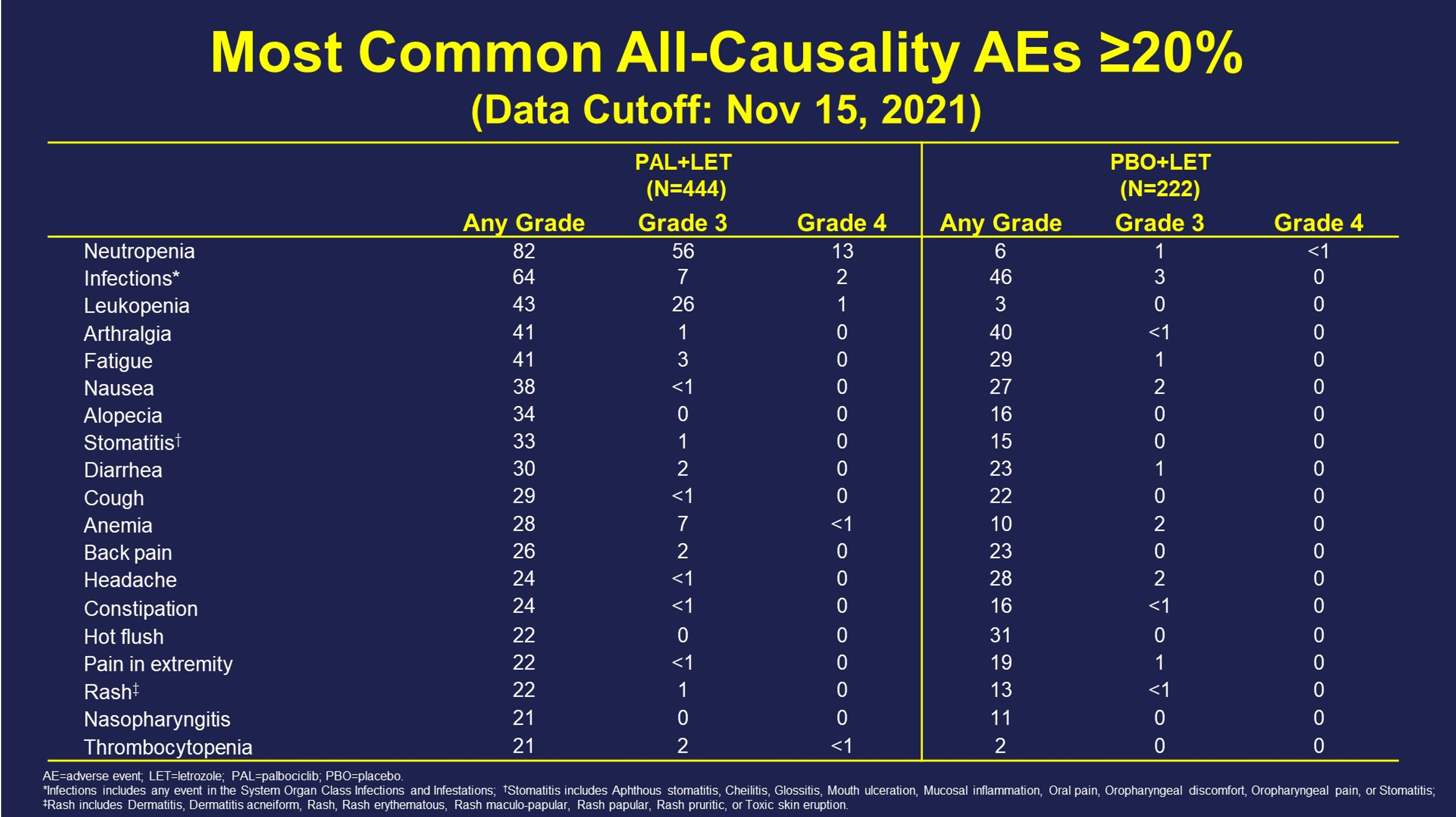
未观察到新的安全信号。
PALOMA-2达到改善PFS的主要终点,但未达到改善OS的次要终点。相比PBO+LET,接受PAL+-LET治疗的患者在数值上OS更长,但结果无统计学意义。
原文来源:
https://meetings.asco.org/abstracts-presentations/208020/video
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CDK4#
40
#ASC#
35
#抑制剂#
40
#CDK#
45
#CDK4/6#
39