J Invest Dermatol:IL-17A产生细胞在皮肤炎性疾病中的调节
2021-10-26 医路坦克 MedSci原创
本文就T淋巴细胞和其他免疫细胞产生的IL-17A家族细胞因子及其在皮肤致病反应中的作用作一综述。在本研究中,我们讨论了与IL-17家族、辅助型T细胞(Th)17细胞和调节性T细胞(Treg)相互作用

IL-17家族细胞因子IL-17A是被称为CTLA-8的CTLA家族蛋白中的一员,并从活化的T细胞中克隆出来,但其在自身免疫发病机制中的作用直到21世纪初才显现出来。它与IL-17B、IL-17C、IL-17D、IL-17E/IL25和IL-17F等6个家族成员具有高度的结构同源性。在生理微生物刺激下,CD4-T细胞(即Th17细胞)中IL-17的表达上调,这导致了微生物诱导的慢性IL-17表达可能是感染诱导的免疫病理学的一个重要组成部分的假设。
Th17和Tregs在抗真菌宿主防御和炎症中的作用
白色念珠菌是一种二相性真菌,它无症状地定植在大约60%的个体上,但当宿主防御减弱时就有可能致病。Toll样受体(Toll-like receptor,TLR),如TLR2和TLR4,以及C型凝集素受体Dectin-1和-2,分别识别磷脂甘露聚糖、O-连接甘露聚糖、葡聚糖和甘露糖残基。在假丝酵母菌作用下,TLR2和Dectin-1激活CARD9-Bcl10Malt1/NF-kB或CARD9/caspase-1依赖的炎症体通路。这些途径有助于Th17诱导的细胞因子的分泌,包括IL-23、IL-6和IL-1b这些都是控制念珠菌所需的。IL-17A在FOXP3阳性和阴性的CD4T细胞亚群中表达上调,表明产生Th17和IL-17A的FOXP3塔细胞(Treg17)在皮肤念珠菌感染过程中的功能相关性。IL-17和IL-22之间的协同作用通过促进中性粒细胞募集和诱导抗菌肽(AMPs)的产生来促进屏障功能,这表明在没有其他慢性炎症刺激的情况下,IL-17提供了基线免疫监视。然而,释放的细胞因子超过最佳水平可能会导致皮肤发生病理变化,这突显了调节Th17反应的必要性。
Tregs在假丝酵母菌感染过程中通过以下两种方式起到保护作用:
1. 在IL-6水平较高的感染早期,Treg通过消耗Th17细胞产生的IL-2来抑制IL-2水平。由于IL-2和IL-15等γ链细胞因子是IL17A表达的负调控因子,导致这些细胞因子减少的Treg的存在增强了IL-17A的产生和宿主防御。在这一阶段,由于IL-6的存在,Tregs还短暂下调了FOXP3的表达。
2.在IL-6水平下降的后期,Tregs降低了Th17细胞的活性和表达TNF-α的Th17细胞,这似乎控制了免疫病理学。Tregs在调节念珠菌感染介导的免疫病理学中的功能重要性从念珠菌病期间Treg活性受损引起的明显炎症中得到了证明。在后期,Treg介导的Th17增强独立于IL-2的消耗,需要TGFb,但Th17细胞中延迟的TNF-a抑制模式尚不清楚。
总的来说,人类突变证明了Th17细胞和Treg在控制念珠菌感染和适当的免疫调节方面的功能重要性,如果没有这些调节,它们可能会进展为念珠菌依赖型慢性炎症。
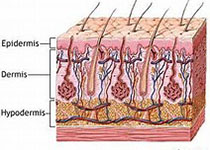
IL-17在银屑病中的作用
银屑病中的IL-23/IL-17信号和免疫调节是一种常见的多基因慢性炎症性皮肤病,IL-17细胞因子的过度表达和IL-23信号的夸大,以及其他上下文促炎信号,被证明会加剧银屑病。从机制上讲,银屑病涉及假定的自身抗原,如AMP LL-37、黑素细胞来源的ADAMTSL5、新脂类抗原PLA2G4D以及角蛋白17。因此,通过浆细胞样树突状细胞的自炎信号导致IFN-a、IFN-g和TNF-α的产生,激活髓样DC产生IL-23并促进T细胞的募集,导致T细胞中IL-17A和IL-22的增加,中性粒细胞的募集,以及表皮微脓肿的形成。
除了中性粒细胞募集,IL-17还增加趋化因子,如CCL20、CXCL8或CXCL1,以及基质金属蛋白酶和AMP,包括DEFB4A,以及S100蛋白A8/A9和A7。IL-17和皮肤角质形成细胞(KCs)之间的额外相互作用可能由产生IL-17的CD8塔T细胞(Tc17)水平升高而局部刺激。Tc17在银屑病皮肤中频率的增加表明,Tc17细胞在自身抗原相遇后可能会扩张。
综上所述,KC炎症反应的自我维持放大导致了观察到的表皮增生以及白细胞亚群的增加,这些细胞亚群提供了更多的细胞因子/趋化因子燃料;因此,KC的不受抑制的增殖实际上是涉及IL-17和其他细胞因子的恶性循环的原因和结果。大量的大规模银屑病GWAS将IL-23/Th17信号轴与银屑病易感性联系在一起。IL-23的两个亚单位内的银屑病相关等位基因以及IL-23受体、NF-kB信号适配器TRAF3IP2和KC特异性下游信号靶IL-17信号靶NFKBIZ及其与银屑病风险的关系突出了IL-17在银屑病发病机制中的中心作用。
从银屑病患者中分离出的Treg功能失调,不能抑制CD4T细胞的增殖,这一观察结果得到了其他研究小组的证实。导致这种功能缺陷的潜在机制包括IL-6和TNF-α增加以及腺苷信号转导减少,这些观察结果的总和支持了Treg功能障碍在维持和加重人类银屑病方面发挥的重要作用,
结论:IL-17细胞因子的适当表达和调节是协调区室化皮肤免疫和调节皮肤炎症病理的核心。结合维持皮肤共生耐受的能力,Treg/Th17/Treg17分化和功能的复杂平衡清楚地协调皮肤炎症发病机制。这些细胞的比例而不是它们的绝对数量和频率的平衡,而这些绝对数量和频率又由细胞因子环境和常驻微生物群维持,似乎决定了促炎触发因素与最佳免疫反应结果。系统评估这些比率并确定协调这种平衡的机制目标将为治疗皮肤炎症疾病及其伴随的合并症提供新的治疗途径。
文献来源:Pandiyan P, McCormick TS,Regulation of IL-17A-Producing Cells in Skin Inflammatory Disorders.J Invest Dermatol 2021 Sep 21
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#EST#
31
#炎性疾病#
36
#IL-17#
45
#IL-17A#
35
#IL-1#
34