Development Cell:乳腺癌细胞利用外囊泡“对话”挟持正常细胞
2020-08-18 Lauren 转化医学网
导言:乳腺癌是全球癌症相关死亡的第二大原因,也是女性最常见的侵袭性癌症类型。在过去的二十年中,乳腺癌的死亡率下降显著,这主要得益于早期发现以及治疗方式的改善。然而,乳腺癌细胞究竟是如何侵袭周围正常细胞
导言:乳腺癌是全球癌症相关死亡的第二大原因,也是女性最常见的侵袭性癌症类型。在过去的二十年中,乳腺癌的死亡率下降显著,这主要得益于早期发现以及治疗方式的改善。然而,乳腺癌细胞究竟是如何侵袭周围正常细胞的还尚不明确,最近发表在《发育细胞》上的一项研究有了新进展。
细胞外囊泡由细胞分泌到细胞外,通常情况下起到细胞间通讯的作用。特别是对于肿瘤来说,细胞外囊泡的分泌不但使肿瘤细胞能够逃逸免疫抓捕,并且具有改善远端肿瘤转移微环境等作用。因此,细胞外囊泡受到越来越多学者的关注。
根据威斯塔研究所(The Wistar Institute)的一项研究,乳腺癌细胞缺氧时发出的信息会导致周围正常上皮细胞发生癌变。这些信息被包装成一种叫做细胞外囊泡(EVs)的颗粒,并在受体正常细胞内对线粒体的形状和位置进行重新编程,最终解除组织形态形成。这些发现发表在《发育细胞》(Developmental Cell)杂志上。
威斯塔研究所的癌症中心主任、罗伯特和佩妮福克斯特聘教授、该研究的第一作者Dario C. Altieri博士表示,“众所周知,癌细胞一直在和邻近的正常细胞“对话”,这对促进癌症进展很重要。癌症进展如何发生的,是什么信号从一个细胞转移到另一个细胞仍然是一个悬而未决的问题。更好地理解这一过程可能会给我们提供重要线索,让我们了解肿瘤是如何劫持附近的正常细胞以促进疾病复发的。”
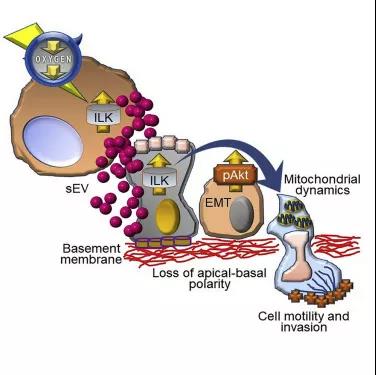
图解摘要
在他们的研究中,Altieri团队在低氧环境中培养乳腺癌细胞,以模拟缺氧状态,这是大多数实体肿瘤周围微环境的标志,并研究这些细胞释放的细胞外囊泡(EVs)。
EVs是一种被包裹在双膜层中的微小结构,由大多数细胞释放,将不同的分子和信息传递给其他细胞。因此,囊泡是细胞间通信的重要手段。在这项研究中,研究人员将重点放在30到150纳米的小型EVs上。
为了分析癌细胞产生的小型细胞外囊泡(sEVs)对邻近正常细胞的影响,研究人员在正常乳腺上皮细胞中培养缺氧状态下细胞释放的sEVs。他们观察到正常受体细胞在培养液中迁移能力的增强,这反过来与线粒体重新分布到细胞外周有关。这与Altieri实验室之前描述的线粒体在支持细胞运动中的作用是一致的。
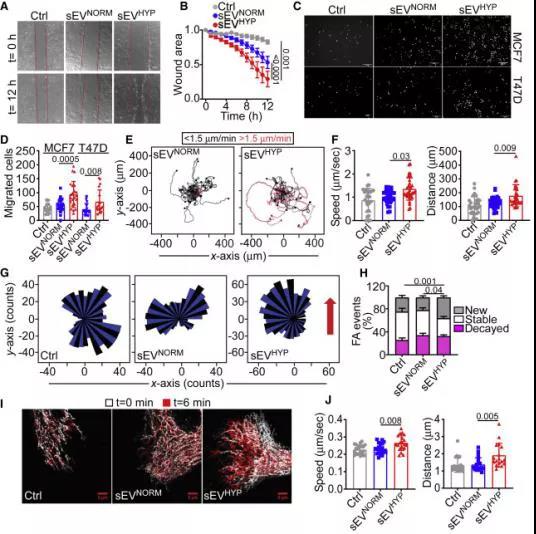
乳腺癌来源的低氧sEVs (sEVHYP)刺激正常乳腺上皮细胞运动
Altieri和他的同事进一步确认整合素连接激酶(ILK)是包装在sEVs中的主要信号转导成分,负责线粒体改变和受体细胞迁移的增加。
反过来,ILK信号的激活深刻影响正常组织形态形成。正常乳腺发展使用三维细胞模型,研究小组发现,使用正常的乳腺发展的3-D模型,研究团队从缺氧癌细胞会产生sEVs,这会导致正常乳腺结构的断裂且诱导肿瘤转移的多种特征,包括形态学改变、细胞增殖失控、细胞死亡减少和上皮-间充质转化(EMT)标记的出现,这一过程赋予癌细胞移动性和从原发部位迁移的能力。
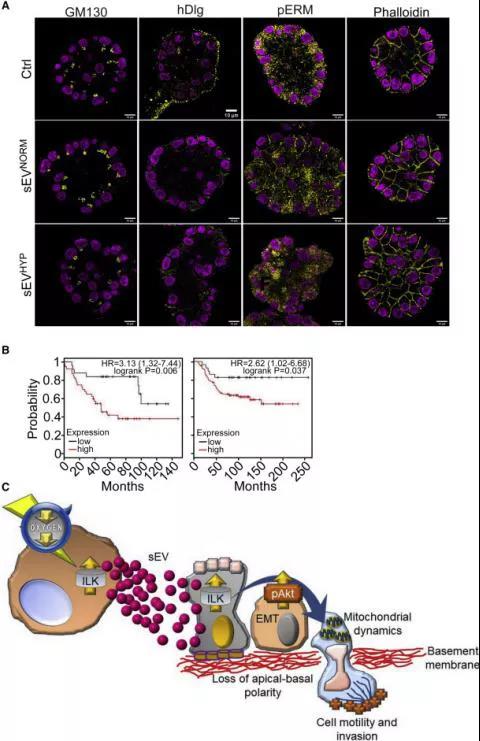
sEVHYP-ILK信号通路在乳腺转化中的作用
Altieri实验室的博士后研究员、该研究的第一作者艾琳·贝托里尼(Irene Bertolini)博士表示:“我们的发现表明,乳腺癌细胞可能使用sEVs来引发局部和远处的疾病进展。基于这些观察,我们认为ILK或线粒体重编程的治疗靶向可能提供新的策略,以中断微环境中这些致瘤前的变化。”
原始出处:
Irene Bertolini, Jagadish C. Ghosh, Andrew V. Kossenkov, et.al. Small Extracellular Vesicle Regulation of Mitochondrial Dynamics Reprograms a Hypoxic Tumor Microenvironment. Development Cell August 10, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Dev#
43
#CEL#
30
不错,用正常乳腺3d模型验证很亮眼
70
#Cell#
32
#癌细胞#
37
#囊泡#
37
👍🏻
85
赞
83