乳腺癌是女性最常见的恶性肿瘤,据估计2018年全球共确诊了200万新发病例。虽然已经进行了广泛的研究,但几乎没有确定什么饮食风险因素会导致乳腺癌。在过去几十年里,反式脂肪酸(TFA)对乳腺癌风险的影响一直存在争议。

富含反式脂肪酸的食物:饼干、薯条、爆米花、奶油蛋糕、奶油冰激凌、代可可脂巧克力、乳饮料、奶茶、蛋黄派等
目前,已假定TFA可影响乳腺癌的风险。但是,研究这种关系的前瞻性研究相对较少,根据激素受体定义的分子亚型、绝经状态和体型的强有力的分析也很少。
在欧洲癌症与营养前瞻性调查(EPIC)中,Matta等在318,607名女性中分析了膳食中TFA(工业反式脂肪酸[ITFA]和反刍动物类反式脂肪酸[RTFA])的摄入量与乳腺癌风险的关系。
反式脂肪酸与乳腺癌风险的相关性
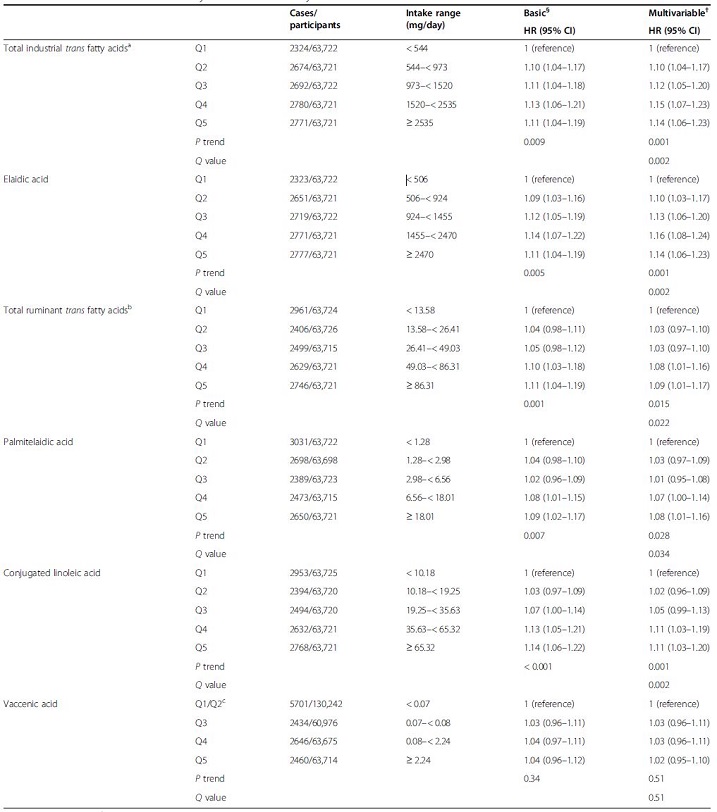
中位随访了8.1年后,共发生了13,241例乳腺癌。在多变量调整模型中,ITFA摄入总量高与乳腺癌风险增加相关(最高五分位 vs 最低五分位的HR为1.14,95%CI 1.06~1.23;P=0.001)。反油酸(主要类型的ITFA)摄入与乳癌风险之间也发现了类似的正相关关系(最高五分位 vs 最低五分位的HR为1.14,95%CI 1.06~1.23;P=0.001)。
RTFA总摄入量也与乳腺癌风险增加相关(HR 1.09,95%CI 1.0 1~1.17;P=0.015)。就单个RTFA而言,研究人员发现两种饮食脂肪酸(共轭亚油酸 HR 1.11,P=0.001;棕榈酸HR 1.08, P=0.028)摄入与乳腺癌风险呈高度正相关。
根据绝经状态、体重指数和乳腺癌亚型校准,ITFA和RTFA总摄入量与乳腺癌风险有类似的相关性。
综上,本研究结果支持TFA与乳腺癌风险相关的假设,即饮食中高ITFA摄入量,特别是反油酸的摄入量,与乳腺癌风险增加有关。
原始出处:
Matta, M., Huybrechts, I., Biessy, C. et al. Dietary intake of trans fatty acids and breast cancer risk in 9 European countries. BMC Med 19, 81 (2021). https://doi.org/10.1186/s12916-021-01952-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#乳腺癌风险#
45
#相关性#
36
#癌风险#
32
#BMC#
31
#反式脂肪#
46
#Med#
27