BMJ子刊:妊娠期服用二甲双胍与子代长期不良预后的风险
2022-01-14 MedSci原创 MedSci原创
妊娠期接触二甲双胍(单独或联合使用胰岛素)并没有增加子代长期不良预后的风险。
二甲双胍是治疗2型糖尿病(T2DM)的一线用药,也是全球T2DM最常用的处方药。虽然二甲双胍没有批准用于孕妇的适应症,但越来越多的妊娠糖尿病 (GDM)患者开始使用二甲双胍治疗。在患有多囊卵巢综合征 (PCOS) 的女性中,二甲双胍通常用来改善无排卵和受孕,一些证据还表明,如果一直服用二甲双胍持续到妊娠期,妊娠不良结局的风险会降低。本研究旨在调查孕妇孕期接触二甲双胍是否增加儿童长期和短期不良后果的风险。
这项来自芬兰的队列研究包括2004-2016年出生的独生子女,他们的母亲怀孕时曾暴露于二甲双胍或胰岛素。主要结局是后代肥胖、低血糖、高血糖、糖尿病、高血压、多囊卵巢综合征、运动及社会发展方面受挫。在一项敏感性分析中,主要结果仅在患有妊娠期糖尿病的儿童中进行调查。次要结果是出生时的不良结果。以胰岛素为参考,采用治疗加权逆概率(IPTW)进行分析。
在主要或敏感性分析中可以看到,与胰岛素相比,二甲双胍或联合治疗并不增加长期预后风险。在次要结果中,二甲双胍的小于胎龄(SGA)风险增加,联合治疗可增加大于胎龄儿、早产和低血糖的风险。未观察到新生儿死亡、高血糖或重大先天性异常的风险增加。
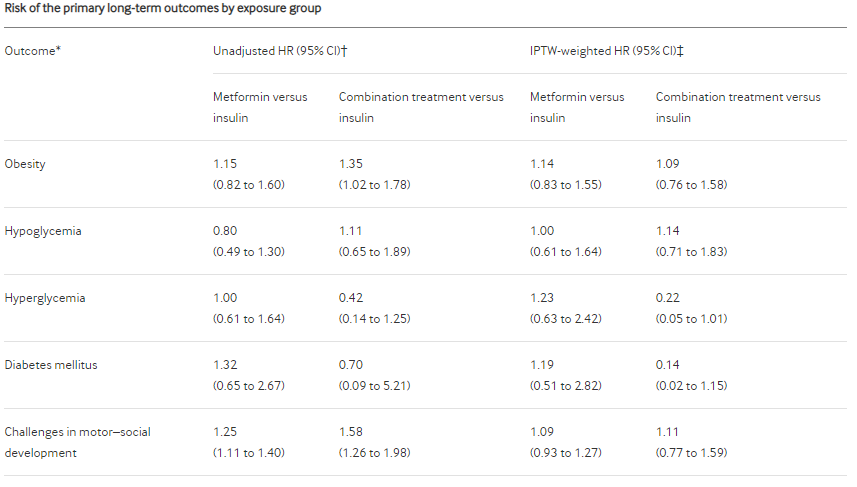
对照组主要长期结果的风险

对照组次要不良结局的风险
总的来说,这项研究发现,与胰岛素相比,妊娠期接触二甲双胍(单独或联合使用胰岛素)并没有增加子代长期不良预后的风险。二甲双胍可能增加SGA的风险,因此有胎儿营养不良风险的孕妇要谨慎使用。
参考文献:Brand KMG, Saarelainen L, Sonajalg J, et al Metformin in pregnancy and risk of adverse long-term outcomes: a register-based cohort study BMJ Open Diabetes Research and Care 2022;10:e002363. doi: 10.1136/bmjdrc-2021-002363
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BMJ#
34
#子代#
55
赞。
49
学习
79
#妊娠期#
41
#不良预后#
44