Nat Commun:HER2阳性乳腺癌在双HER2阻断期间和之后的表型变化
2020-08-01 MedSci原创 MedSci原创
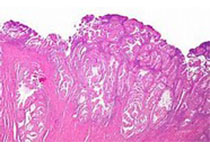
HER2阳性(HER2+)乳腺癌内的HER2富集型(HER2-E)亚型高度依赖HER2通路。然而,20-60%的HER2+/HER2-E肿瘤在抗HER2疗法后不能达到完全反应。在此,我们评估了PAME
HER2阳性(HER2+)乳腺癌内的HER2富集型(HER2-E)亚型高度依赖HER2通路。然而,20-60%的HER2+/HER2-E肿瘤在抗HER2疗法后不能达到完全反应。在此,我们评估了PAMELA试验的HER2+/HER2-E肿瘤和乳腺癌细胞系新辅助治疗前、治疗期间和治疗后的基因表达数据。
结果显示,HER2-E疾病的双重HER2阻断在患者的肿瘤和体外模型中都会诱导出低增殖的Luminal A表型。与HR阴性疾病相比,这些生物学变化在激素受体阳性(HR+)疾病中更为明显。有趣的是,用抗HER2治疗增加瘤体表型,增加了对CDK4/6抑制的敏感性。最后,在体外停止HER2靶向治疗,或对抗HER2治疗的获得性耐药,会导致原有HER2-E表型的恢复。
总之,该研究结果支持使用维持性抗HER2治疗和利用CDK4/6抑制进行亚型切换的治疗方法。
原始出处:
Fara Brasó-Maristany, Gaia Griguolo, et al., Phenotypic changes of HER2-positive breast cancer during and after dual HER2 blockade. Nat Commun. 2020 Jan 20;11(1):385. doi: 10.1038/s41467-019-14111-3.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#COMMUN#
39
#阻断#
32
#Nat#
24
学习
71
#HER2阳性#
27
#表型#
32