J Gastroenterology:炎症性肠病患者动静脉血栓栓塞导致的死亡率和风险因素分析
2021-10-15 MedSci原创 MedSci原创
炎症性肠病 (IBD) 是一种慢性复发性肠道和全身炎症性疾病,有两种主要的表型:溃疡性结肠炎 (UC) 和克罗恩病 (CD)。而血栓栓塞(TE)是一种严重的肠
炎症性肠病 (IBD) 是一种慢性复发性肠道和全身炎症性疾病,有两种主要的表型:溃疡性结肠炎 (UC) 和克罗恩病 (CD)。而血栓栓塞(TE)是一种严重的肠外表现,来自西方国家的大规模队列研究表明,IBD 患者静脉血栓栓塞 (VTE) 的发生率是非 IBD 对照组的两到三倍。近年来,一些报告表明,与非 IBD 患者相比,IBD 患者发生动脉血栓栓塞 (ATE) 的风险明显增加,包括容易出现缺血性心脏病 (IHD) 和脑血管疾病 (CVD),一项跨国研究显示,住院 IBD 患者的 VTE 发生率是非 IBD 对照组的 2.27 倍,而在亚洲国家没有关于 IBD 患者 TE 相关严重程度和死亡的发生率和危险因素的大规模全国性研究报告,因此,本研究旨在揭示IBD 患者TE 的死亡率和危险因素。

在 31940 名 IBD 患者中,TE 的发生率为 1.89%。在 IBD 和 TE 合并 IBD 患者中,严重 TE 和 TE 相关死亡率的频率分别为 10.7% 和 1.0%。严重 ATE 和 ATE 相关死亡的唯一危险因素是缺血性心脏病。严重 VTE 和 VTE 相关死亡的独立危险因素是年龄(≤ 45 岁)、VTE 部位和疾病严重程度,抗 TNF 治疗是潜在的负面危险因素。严重 VTE 患者发生持续性VTE 和后遗症的风险很高。

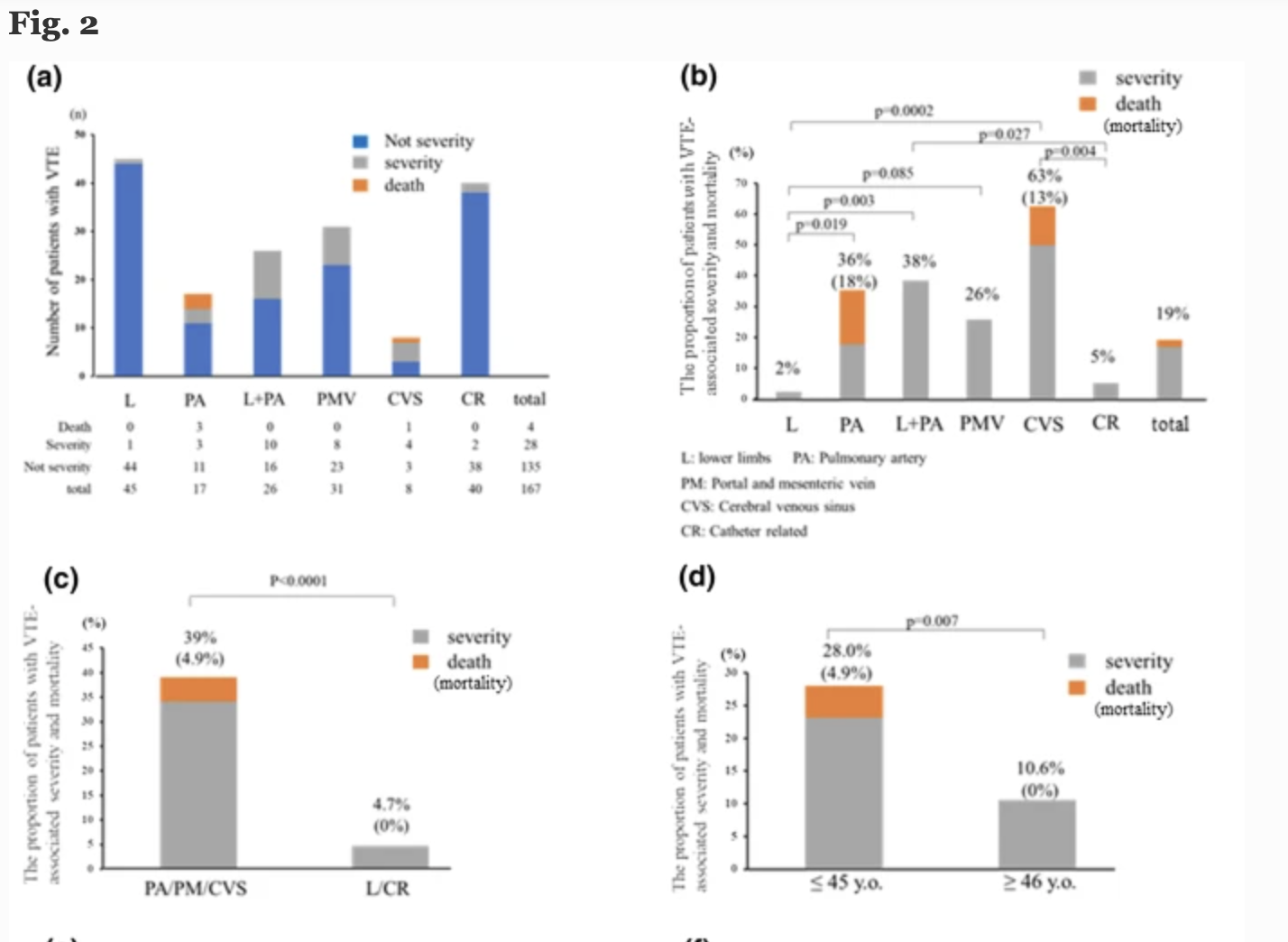
众所周知,心血管疾病(CVS)与年轻患者的严重程度和死亡风险最高有关。在年轻患者肺动脉栓塞和 PMV 的比例升高,而与 ATE 不同,亚洲和西方国家的IBD患者的VTE发生率相当。亚洲IBD患者迫切需要IBD相关 TE 的治疗和预防策略。
原始出处 :
Katsuyoshi Ando. Et al. A nationwide survey concerning the mortality and risk of progressing severity due to arterial and venous thromboembolism in inflammatory bowel disease in Japan. Journal of Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Gastroenterol#
37
#AST#
44
#静脉血#
46
#GAS#
43
#静脉#
31
学习了,谢谢
64
#Gastroenterology#
34
#炎症性#
34
#炎症性肠病患者#
27