Gastric Cancer:晚期胃癌中二线化疗中早期肿瘤应答和生活质量的关系:ABSOLUTE研究的更新
2021-06-29 yd2015 MedSci原创
晚期胃癌二线应用紫杉类化疗,早期的肿瘤退缩跟生活质量的维持有关。
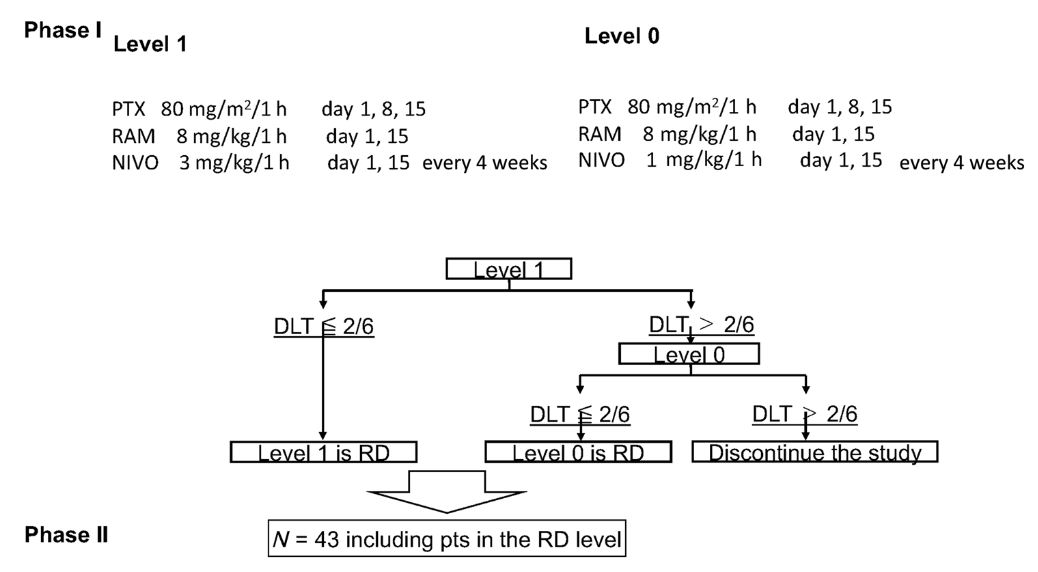
在全球范围内,胃癌是第五大最常见的恶性肿瘤,是癌症相关死亡的第三大主要原因。晚期胃癌的预后是令人沮丧的。晚期胃癌的标准治疗是化疗,氟嘧啶联合铂类仍是标准一线化疗。直到最近,对于难治性或不耐受一线化疗的患者的二线化疗是溶剂型(Sb)紫杉醇(PTX)、多西他赛和伊立替康。然而,Sb-PTX可引起部分患者的超敏反应和过敏反应,这可能与Sb-PTX中存在的聚乙氧基蓖麻油有关。而纳米白蛋白结合型紫杉醇在不使用预处理的情况下可将相关过敏的风险降至最低。 ABSOLUTE试验(编号:JapicCTI-132059)是日本开展的一项随机、开放、非劣效性的3期试验,评估白蛋白结合型紫杉醇(nab-PTX)对比溶媒型紫杉醇(Sb-PTX)二线治疗晚期胃癌的疗效。前期结果分析证实nab-PTX非劣效于Sb-PTX。近期,该研究在Gastric Cancer杂志上更新了数据,分析早期肿瘤应答跟生活质量(HRQOL)的关系。
使用EuroQol-5 Dimension (EQ-5D) 评分来评估第8周是肿瘤应答(CR + PR and PD)患者的生活质量,评估肿瘤恶化时间(TtD)。最小的重要差异(MID)认为是0.05。每周nab-PTX治疗组和每周Sb-PTX治疗组中分别有143 和160 例患者可评估疗效。
其中nab-PTX组中的142例患者,在第8周时分别有41例(28.9%),68例(47.9%)和33例(23.2%)获得完全缓解(CR)+ 部分缓解(PR)、疾病稳定(SD)以及疾病进展(PD)。而Sb-PTX组中的159例患者,在第8周时分别有29例(18.2%), 86例(54.1%), 和44例(27.7%)完全缓解(CR)+ 部分缓解(PR)、疾病稳定(SD)以及疾病进展(PD)。
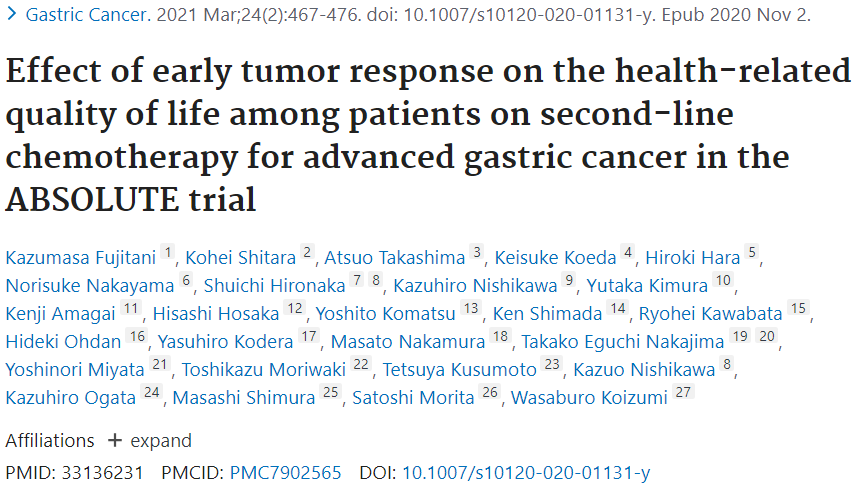
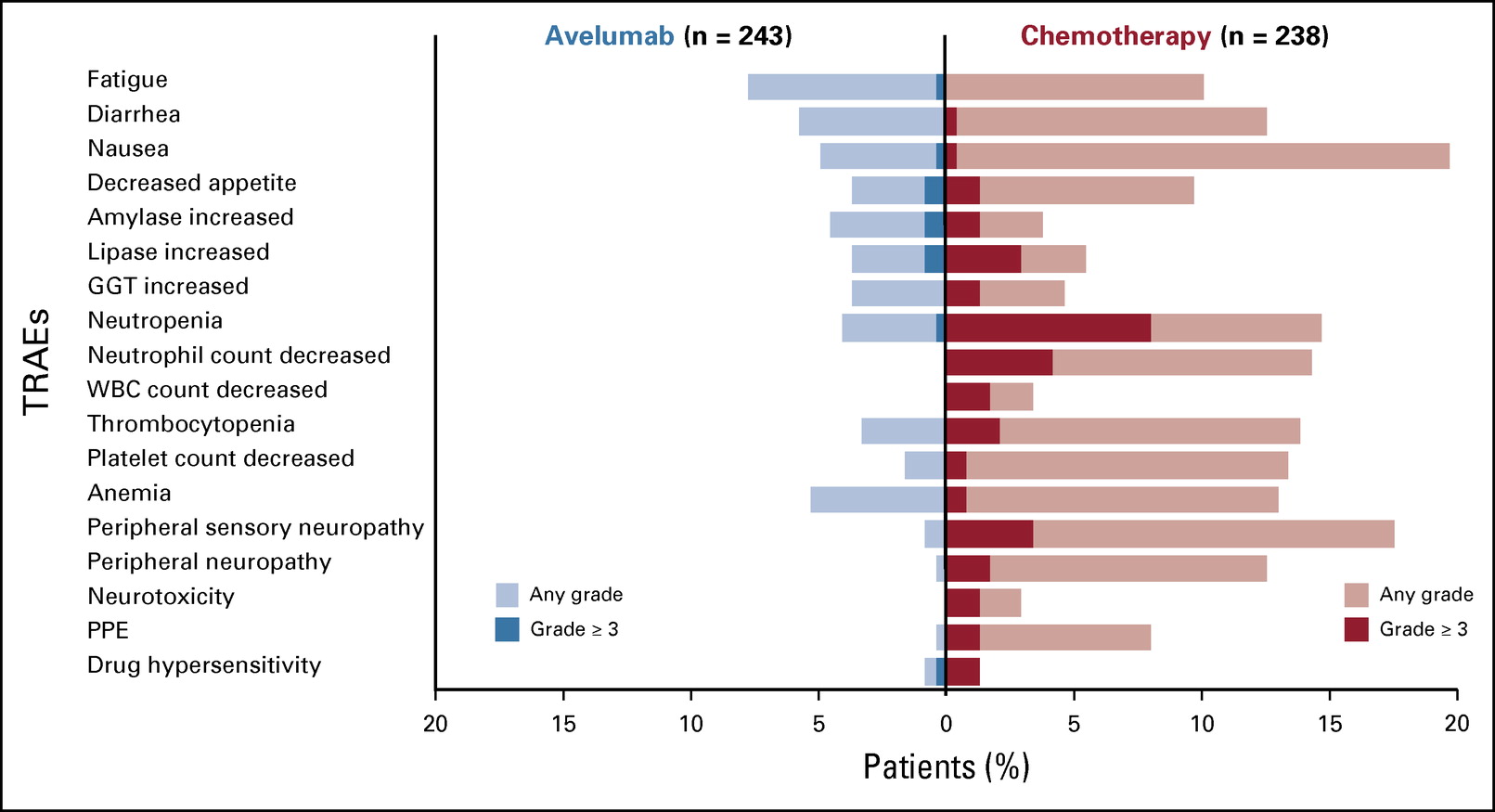
nab-PTX组中的CR+PR和PD患者,从基线到第8周的EQ-5D评分为0.0009 和 − 0.1229 (95% CI, 0.0294–0.2182);而Sb-PTX组中的CR+PR和PD患者,从基线到第8周的EQ-5D评分为− 0.0019 和 − 0.1549 (95% CI, 0.0507–0.2553)。两组中CR+PR患者较PD患者获得更好的EQ-5D评分。
生活质量评分
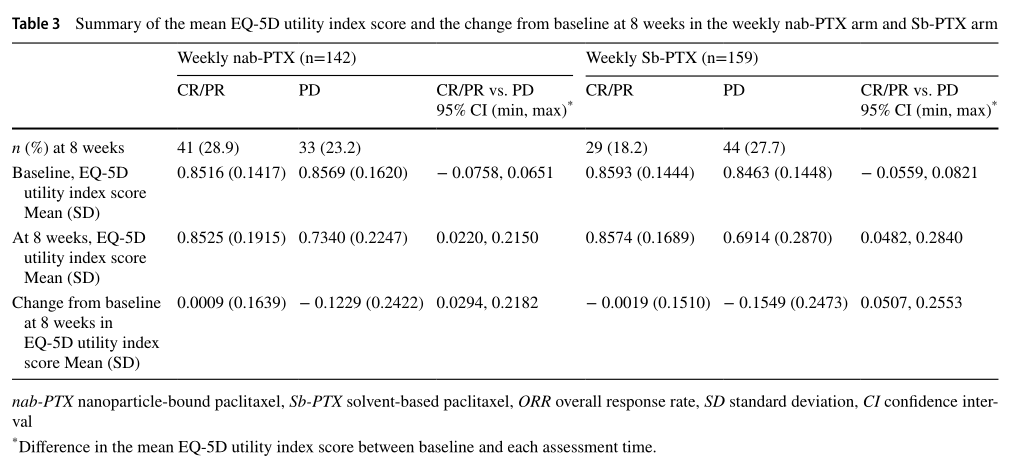
nab-PTX组的41例CR + PR患者中有11例(26.8%)和Sb-PTX组的29例CR + PR患者中有7例(24.1%),从基线到第8周的EQ-5D评分超过MID。两组中近三分之一的CR+PR患者的生活质量得到改善或没有变化。另外,nab-PTX组的33例PD患者中有16例(48.5%)和Sb-PTX组的44例CR + PR患者中有24例(54.5%),从基线到第8周的EQ-5D评分超过MID。两组中约一半PD患者的生活质量恶化。
MID
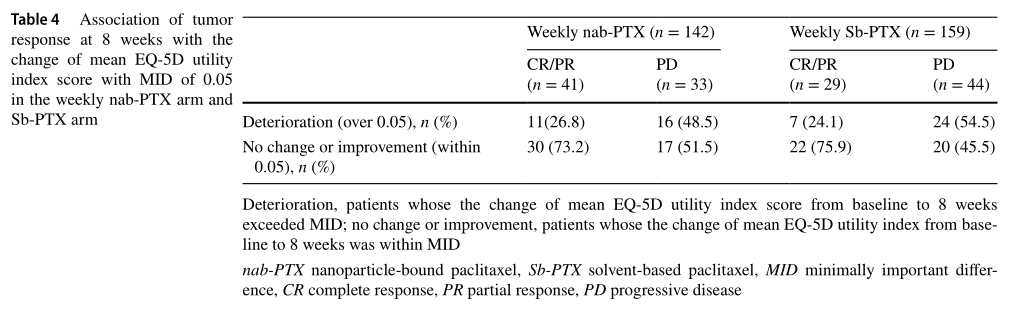
nab-PTX组中CR+PR和PD患者的中位TtD时间分别为3.9和2.2个月(HR=0.595, 95% CI 0.358–0.989);而Sb-PTX组中CR+PR和PD患者的中位TtD时间分别为4.7和2.0个月(HR= 0.494,95% CI 0.291–0.841)。两组中CR+PR患者的中位TtD时间均较PD患者延长。
两组的TtD
综上,晚期胃癌二线应用紫杉类化疗,早期的肿瘤退缩跟生活质量的维持有关。
原始出处:
Fujitani K, Shitara K, Takashima A, et al. Effect of early tumor response on the health-related quality of life among patients on second-line chemotherapy for advanced gastric cancer in the ABSOLUTE trial. Gastric Cancer. 2021 Mar;24(2):467-476. doi: 10.1007/s10120-020-01131-y. Epub 2020 Nov 2. Erratum in: Gastric Cancer. 2020 Dec 9;: PMID: 33136231; PMCID: PMC7902565.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#gastric#
52
#AST#
49
#GAS#
53
#晚期胃癌#
37
写的有帮助
62