JAMA Netw Open:医生知识水平越高,阿片类药物开出率越低!
2021-07-03 MedSci原创 MedSci原创
众所周知,阿片类药物(Opioid)作为镇痛的主要类别,在缓解中度至重度疼痛疗效非常显著,尤其是对癌症造成的剧烈疼痛具有良好的效果。同时,阿片类药物在用于麻醉时可有效抑制气管插管和手术疼痛刺激引起的应
众所周知,阿片类药物(Opioid)作为镇痛的主要类别,在缓解中度至重度疼痛疗效非常显著,尤其是对癌症造成的剧烈疼痛具有良好的效果。同时,阿片类药物在用于麻醉时可有效抑制气管插管和手术疼痛刺激引起的应激反应,维持血压、心率的稳定。

WHO
虽然,阿片类药物能缓解疼痛,但在有效控制疼痛方面十分有限,且长期使用与诸多不良反应相关,包括免疫抑制、自我奖惩机制失调和神经激素缺陷等。那么,随着科学家对阿片类药物的深入研究,临床知识的增加是否与阿片类药物处方的减少有关?
近日,发表在JAMA Netw Open杂志上的一项研究显示,在2015年至2017年间,临床知识得分较高的医生减少了阿片类药物处方,当时指南迅速向减少阿片类药物处方的方向转变。
这项横断面研究包括美国10246名中年普通内科医生,比较 2009 年至 2011 年临床知识与阿片类药物处方之间的关联,当时处方在全国达到峰值,而 2015 年至 2017 年指南推荐减少使用阿片类药物处方。
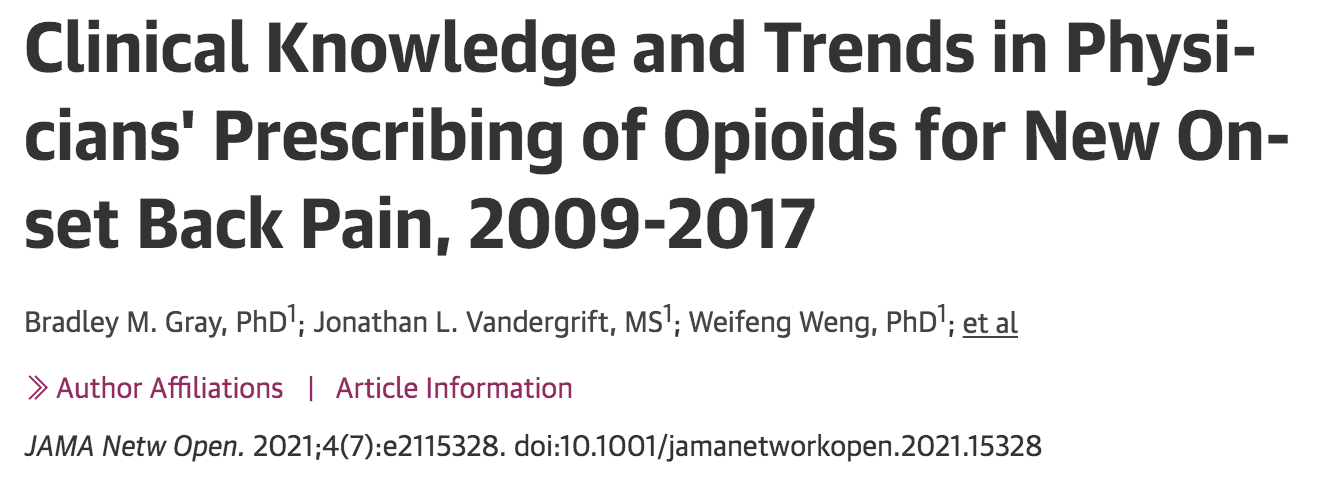
该研究包括了 55 387 次腰痛就诊,其中37185 (67.1%) 次为女性患者,41978 (75.8%) 次为白人患者,患者的平均年龄为 76.2年。任何阿片类药物处方的阿片类药物处方率占 21.6%,高剂量或长时间使用(HDLD) 处方占17.6% 。从 2009 年到 2011 年,最高和最低知识四分位数的医生阿片类药物处方开出率相似,差异为 0.5(95% CI,–1.9 至 3.0)个百分点。 2015 年至 2017 年,与知识水平最低的四分位数医生相比,知识水平最高的四分位数医生开阿片类药物的频率更低(差异为 4.6 个百分点;95% CI,–7.5 至 –1.8 个百分点)。
早期(2009-2011)、中期(2012-2014)和晚期(2015-2017)期间,知识水平与阿片类药物处方之间的关联
综上,医生知识水平与具有临床意义的处方行为有关。知识水平得分高的医生可能对护理标准的变化更加敏感。在 2009 年至 2011 年的早期期间并未观察到这种差异。随着医生知识水平的提升, 2015 年至 2017 年,知识水平得分高的医生开阿片类药物的频率显著降低。
原始出处
Bradley M. Gray, PhD1; Jonathan L. Vandergrift, MS1; Weifeng Weng, PhD1; et al.Clinical Knowledge and Trends in Physicians' Prescribing of Opioids for New Onset Back Pain, 2009-2017.JAMA Netw Open. 2021;4(7):e2115328. doi:10.1001/jamanetworkopen.2021.15328
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
27
#NET#
29
理学指南
66
#阿片类药物#
38
#阿片类#
40
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
53