JAMA Netw Open:COVID-19患者出院后不仅运动耐量降低,心理也受到创伤!
2021-01-30 MedSci原创 MedSci原创
目前,新冠肺炎(COVID-19)仍在全球肆虐,据数据显示,全球已确诊超1亿258万,累计死亡人数超221.4万。
目前,新冠肺炎(COVID-19)仍在全球肆虐,据数据显示,全球已确诊超1亿258万,累计死亡人数超221.4万。自COVID-19大流行以来,各国科学家将注意力集中在COVID-19感染急性期的临床特征和预后上。尽管COVID-19是一种全身性疾病,但对其肺功能及其他后遗症类型和严重性尚不清楚。
近日,发表在JAMA Netw Open杂志上的一项研究发现,出院后4个月,COVID-19患者出现常见的呼吸道,身体和心理后遗症。
研究人员对来自意大利北部的一家医院于2020年3月1日至6月29日出院的767名年龄在18岁以上的患者进行前瞻性队列研究,这些患者均接受了住院治疗。研究人员收集了患者的健康记录,住院期间COVID-19诊断的症状以及并发症(回顾性记录)以及合并症的类型和数量的数据,并在出院后的3-4个月通过电话进行随访。
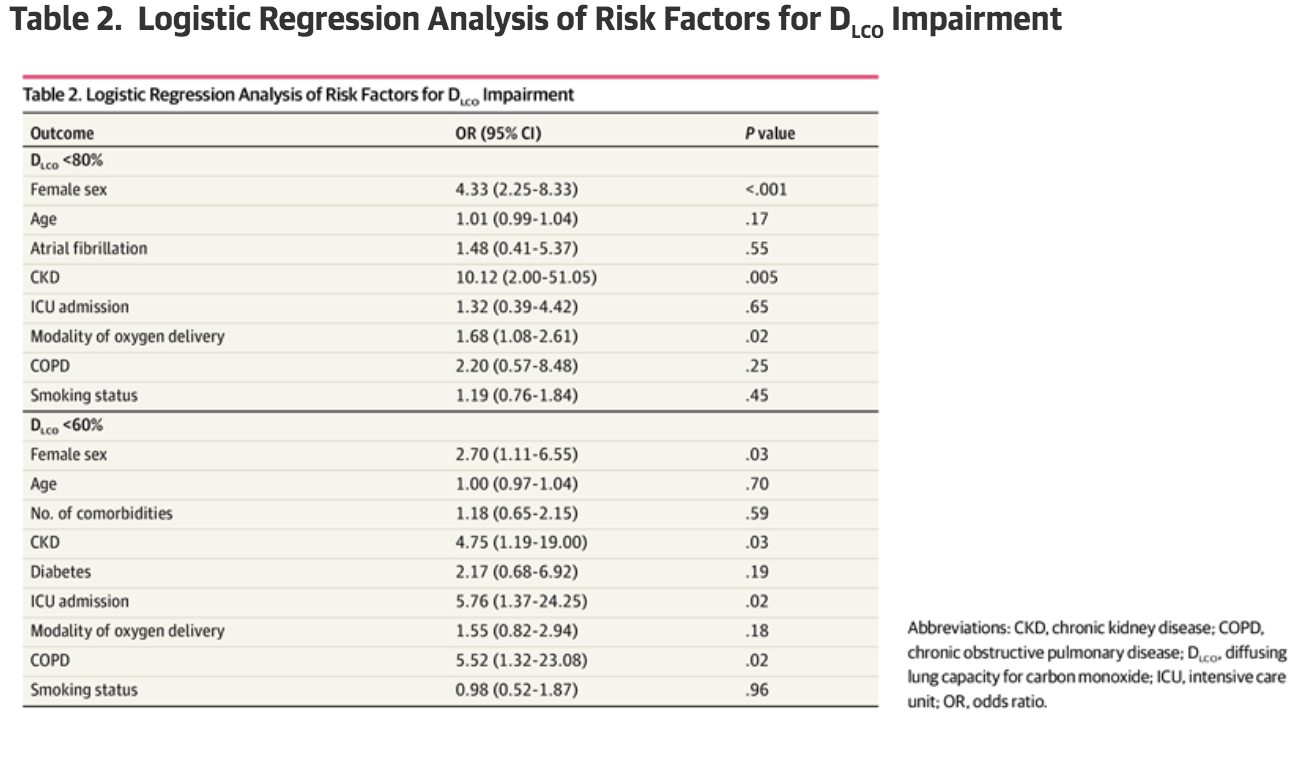
研究结果主要描述了一氧化碳扩散肺容量(Dlco)低于预期值80%的患者比例。次要结果包括严重肺功能损伤患者的比例(定义为Dlco<60%的预期值);创伤后应激症状患者的比例(使用事件影响量表-修订总分测量);功能损伤患者的比例(使用短期体能测试[SPPB]评分和2分钟步行测试评估);以及识别与Dlco减少和心理或功能后遗症相关的因素。
结果显示,在767名因重度COVID-19住院的患者中,494人(64.4%)拒绝参与,35人(4.6%)在随访期间死亡。共有238名患者(31.0%)同意参与此研究。其中,219名患者能够同时完成肺功能检测和Dlco测量。113名患者(51.6%)的Dlco降至估计值的80%以下,34名患者(15.5%)降至60%以下。
 在身体功能方面,根据SPPB测试结果,53名患者(22.3%)活动受限。所有其他患者均接受了2分钟的步行测试,其中75名患者(31.5%)有较轻微的损伤。因此,共有128名患者(53.8%)出现功能障碍,而且有50名患者(21.0%),运动的耐受性恶化。
在身体功能方面,根据SPPB测试结果,53名患者(22.3%)活动受限。所有其他患者均接受了2分钟的步行测试,其中75名患者(31.5%)有较轻微的损伤。因此,共有128名患者(53.8%)出现功能障碍,而且有50名患者(21.0%),运动的耐受性恶化。
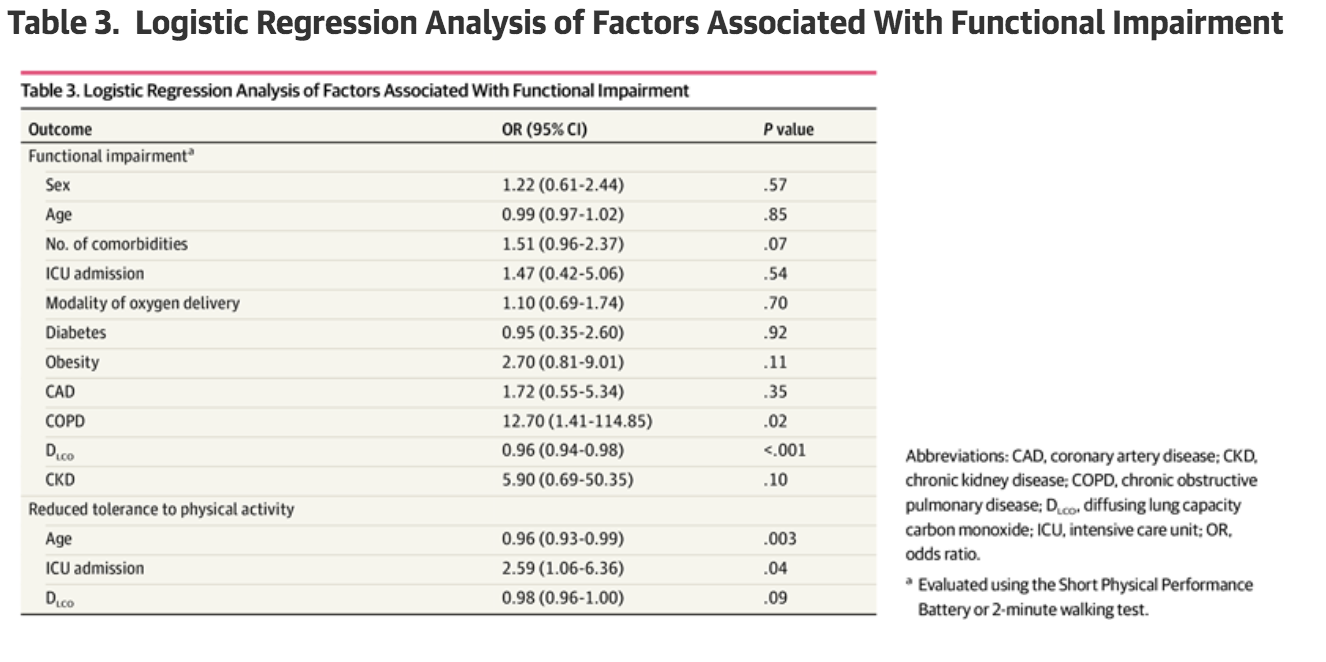
在心理健康方面,约17.2%的COVID-19幸存者出现创伤后应激障碍,而且男性是与PTS症状相关的唯一独立因素。由于该研究的心理评估仅限于PTS症状,无法就COVID-19的整体心理影响得出明确的结论,其中可能包括睡眠障碍,焦虑和抑郁等。
总之,在这项队列研究中,在出院后直至4个月内,仍有很大比例患者与COVID-19相关的症状,其中最常见的是运动耐量降低。此外,COVID-19其他后遗症,例如呼吸和身体功能障碍,可能会影响个体心理健康。肺损伤可能与COVID-19幸存者的生活质量下降有关。
原始出处
Mattia Bellan, MD, PhD; Daniele Soddu, MD; Piero Emilio Balbo, MD; et al.Respiratory and Psychophysical Sequelae Among Patients With COVID-19 Four Months After Hospital Discharge.JAMA Netw Open. 2021;4(1):e2036142. doi:10.1001/jamanetworkopen.2020.36142
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#NET#
32
#PE#
26
#COVID-19患者#
41
#创伤#
34
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
56