Neurology:人工智能,辅助诊断颞叶癫痫
2021-09-06 Freeman MedSci原创
这个预测TLE侧向的模型是以现成的常规MRI对比度为基础的,并提供了比视觉放射学评估更多的准确性
许多药物难治性颞叶癫痫(TLE)患者出现海马体硬化(hippocampal sclerosis ,HS)。MRI有助于识别这种可能形成致痫灶基质的病变,从而简化手术前的评估。
海马硬化的主要影像学特征是海马体积的损失,通常与低密度T1和高密度T2加权信号有关。这些特征的生物学有效性已经通过MRI和组织病理学的联合分析得到证实,表明细胞密度降低和胶质增生分别与萎缩和T2高强化正相关。
然而,在临床实践中,在30-50%有明确的TLE临床电学证据的手术人选中,MRI仍不能显示海马的病变。这一广泛的范围可能部分归因于不理想的成像方案和有限的专业经验。
此外,虽然定量分析,包括海马体积测量、基于体素的形态测量、T2松弛测量( T2 relaxometry)和FLAIR信号强度的测量已被证明比视觉评估更敏感,但它们仍未得到充分利用。值得注意的是,HS的体内特征受神经元缺失和胶质增生的严重程度的影响,以孤立的胶质增生为典型的微妙形式往往能逃避检测。
因此,许多MRI未显示的患者可能要接受颅内脑电图检查,这种检查的风险与切除性手术相似,而且费用很高。
尽管有大量的神经影像学文献评估TLE的海马结构完整性,但绝大多数的研究都是针对群体层面的变化。另一方面,个别分析通常利用单一的对比,将其归一化为健康受试者的分布,很少解决MRI阴性患者的侧重点问题。
藉此,加拿大麦吉尔大学的Benoit Caldairou等人实施一个机器学习框架,依靠现成的常规T1和T2加权对比,对个体患者的HS进行侧向分析。
由于HS的典型特征是T1加权的低密度和T2加权的高密度,他们还通过将FLAIR强度除以T1加权的强度来生成一个合成对比,从而最大限度地提高它们的综合贡献,以检测完整的HS光谱。我们将该分类器应用于TLE中HS的MRI特征,并在两个独立的队列中评估其普遍性。
他们训练了一个基于表面的线性判别分类器(surface-based linear discriminant classifier ),使用T1加权(形态)和T2加权以及FLAIR/T1(强度)特征。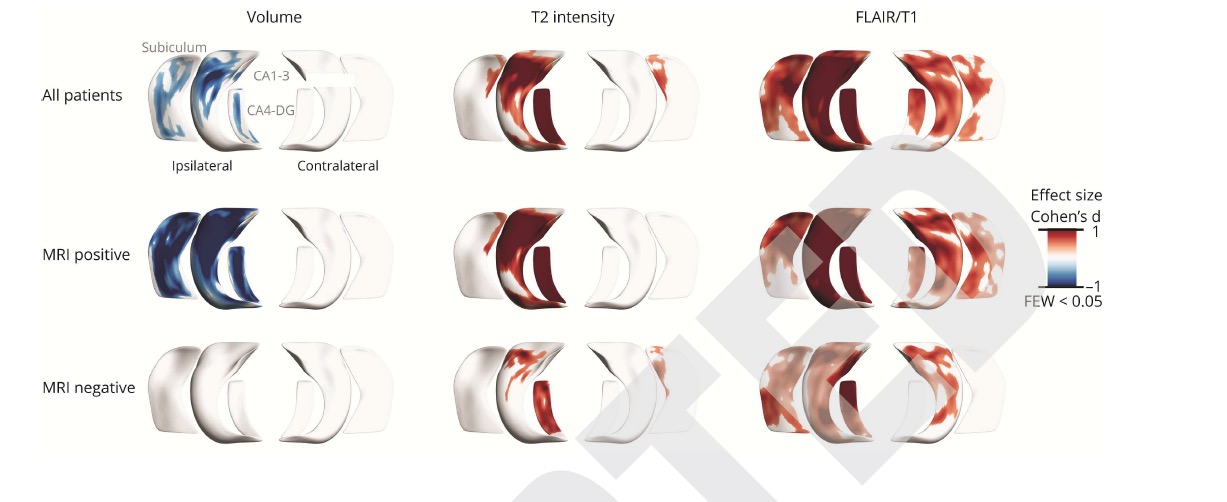
该分类器在60名TLE患者(平均年龄:35.6岁;58%为女性)身上进行了训练,这些患者有组织学证实的海马硬化症(HS)。根据神经放射学读数,42%的病例被认为是MRI阴性的(40%是根据海马体积测定)。
预测模型自动将患者标记为左侧或右侧TLE。侧向的准确性(Lateralization accuracy )与脑电-临床数据进行了比较,包括手术的一侧。在两个独立的TLE队列中进一步评估了分类器的准确性,这些队列具有相似的人口统计学和电临床特征(n=57;58%MRI阴性)。
他们发现:无论HS的在MRI上的可视性如何,总体侧化准确率为93%(95%;CI 92% - 94%)。在MRI阴性的TLE中,T2和FLAIR/T1强度的组合在训练(84%,曲线下面积(AUC):0.95±0.02)和验证队列(队列1:90%,AUC:0.99;队列2:76%,AUC:0.94)中都提供了最高的准确性。
这个预测TLE侧向的模型是以现成的常规MRI对比度为基础的,并提供了比视觉放射学评估更多的准确性。T1加权强度降低和T2加权强度增加的综合贡献使得合成FLAIR/T1对比度对MRI阴性的HS特别有效,为广泛的临床转化奠定了基础。
原文出处:
Caldairou B, Foit NA, Mutti C, et al. An MRI-Based Machine Learning Prediction Framework to Lateralize Hippocampal Sclerosis in Patients With Temporal Lobe Epilepsy. Neurology. Published online September 2, 2021:10.1212/WNL.0000000000012699. doi:10.1212/WNL.0000000000012699
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#Neurol#
34
学习了
49
#颞叶癫痫#
50
学习
66
学习
71
学习了
49