CHEST:支气管扩张加重期间和之后的心血管事件和长期死亡率的关系
2021-10-23 刘少飞 MedSci原创
支气管扩张症是一种会引起支气管发脓、感染的慢性支气管炎症。支气管扩张症患者的临床表现主要为咳嗽、咳血。由于支气管扩张症患者存在反复感染现象,所以此种疾病的病程会比较长,且不可逆转。

支气管扩张症是一种会引起支气管发脓、感染的慢性支气管炎症。支气管扩张症患者的临床表现主要为咳嗽、咳血。由于支气管扩张症患者存在反复感染现象,所以此种疾病的病程会比较长,且不可逆转。在临床上会将支气管扩张症分为加重期、稳定期,在支气管扩张症的急性加重期,患者的肺组织、肺功能损害会更为严重。
那么,支气管扩张症急性加重期与心血管事件及长期死亡率的关系是怎样的呢?
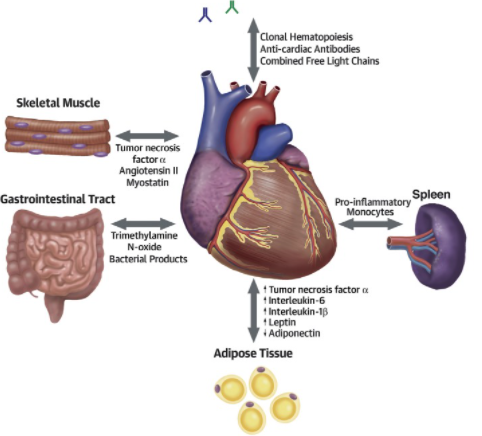
研究背景:基于人群的回顾性研究表明,在支气管扩张症恶化期间和之后,心血管事件(如心律失常、缺血性发作或心力衰竭)的风险会增加。
研究问题:支气管扩张加重期间和之后发生心血管事件 (CVE) 的危险因素及其对死亡率的影响是什么?
研究设计和方法:
对两家三级医院的 250 名支气管扩张患者进行的前瞻性观察研究的事后回顾性分析。每个患者只考虑第一次恶化,收集人口统计学、合并症和严重程度数据。
主要结果是 CVE 的出现和死亡率。使用半竞争风险模型分析 CVE 的风险因素。
研究结果:
在 35 个月的中位随访期间,74 名(29.6%)患者患有 CVE,93 名(37.2%)患者死亡。竞争风险分析表明,年龄、动脉高血压、慢性阻塞性肺疾病以及潜在的严重恶化显着增加了发生 CVE 的风险。与没有 CVE 的患者相比,有 CVE 的患者死亡率更高。
研究启示:人口统计学因素和合并症是支气管扩张急性加重后发生 CVE 的危险因素。 CVE 的出现使长期预后恶化。
文章出处:
Méndez R, Feced L, Alcaraz-Serrano V, González-Jiménez P, Bouzas L, Alonso R, Martínez-Dolz L, Hervás D, Fernández-Barat L, Torres A, Menéndez R. Cardiovascular Events during and after Bronchiectasis Exacerbations and Long-Term Mortality. Chest. 2021 Oct 14:S0012-3692(21)04101-5. doi: 10.1016/j.chest.2021.10.013. Epub ahead of print. PMID: 34656526.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血管事件#
57
#EST#
57
#支气管#
42
#Chest#
44
#扩张#
49