Eur Urol Oncol:雄激素剥夺疗法联合根治性局部治疗与单独的雄激素剥夺疗法治疗新诊断寡转移性前列腺癌的疗效比较
2022-07-16 AlexYang MedSci原创
确定了根治性局部治疗(RLT)是否能提高寡转移性前列腺癌(OMPCa)患者的生存率。
既往的研究表明,男性转移性前列腺癌患者可能从原发肿瘤的局部治疗中获益。

近期,来自上海复旦大学肿瘤中心泌尿外科的研究人员在《Eur Urol Oncol》上发表文章,确定了根治性局部治疗(RLT)是否能提高寡转移性前列腺癌(OMPCa)患者的生存率。
研究为开放标签的随机对照试验,包括了新诊断的OMPCa患者,诊断标准为5个或更少的骨或盆腔外淋巴结转移,且没有内脏转移。
研究人员将患者随机分配接受雄激素剥夺疗法(ADT)或ADT联合RLT。接受RLT的男性行细胞还原性根治性前列腺切除术(RP)或前列腺放射治疗(RT)。研究的主要结果是放射学无进展生存期(rPFS)。次要结果是总生存期(OS)和前列腺特异性抗原(PSA)无进展生存期。
在2015年9月至2019年3月期间,共有200名患者参与并随机分配,每组有100名男性。中位年龄为68岁,诊断时PSA中位数为99纳克/毫升。在研究组中,96名患者接受了RLT(85名RP和11名RT)。在对照组中,17名患者最终接受了RLT(15名RP和2名RT)。所有患者均被纳入意向治疗分析。经过中位数为48个月的随访,研究组未达到中位rPFS,而对照组为40个月(危险比[HR]0.43,95%置信区间[CI]0.27-0.70;p=0.001)。研究组的3年OS率为88%,对照组为70%(HR 0.44,95% CI 0.24-0.81;p=0.008)。
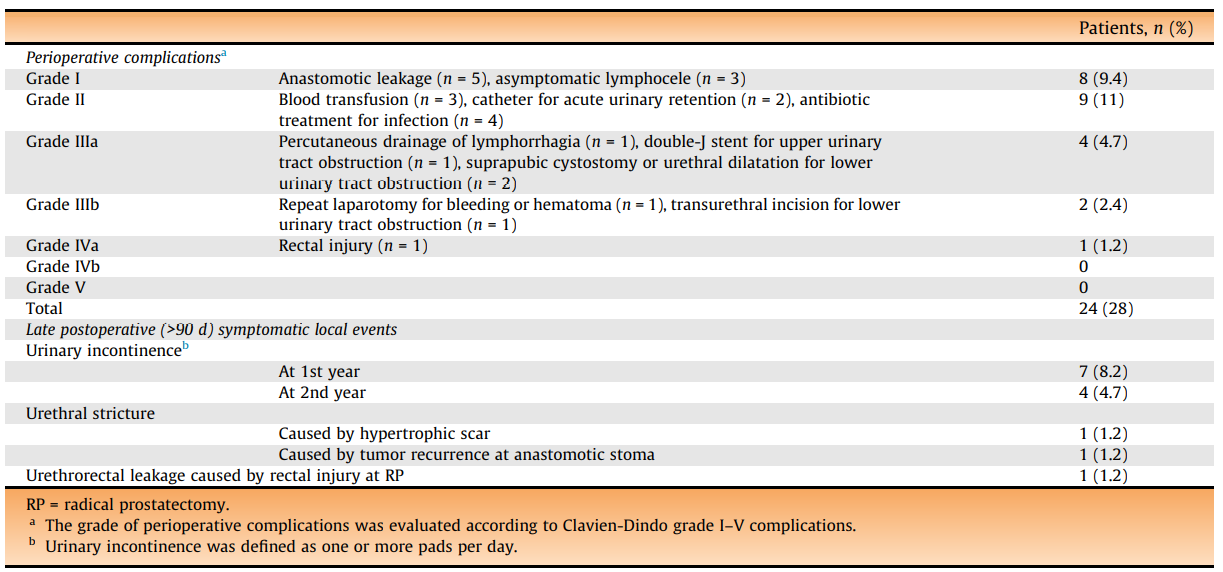
根治性前列腺期切除术治疗患者的围手术期和术后并发症情况
综上所述,新诊断的OMPCa患者接受ADT加RLT(主要是前列腺切除术)的rPFS和OS率均明显高于仅接受ADT的患者。
原始出处:
Bo Dai , Sheng Zhang , Fang-Ning Wan et al. Combination of Androgen Deprivation Therapy with Radical Local Therapy Versus Androgen Deprivation Therapy Alone for Newly Diagnosed Oligometastatic Prostate Cancer: A Phase II Randomized Controlled Trial. Eur Urol Oncol. Jun 2022
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#雄激素剥夺#
0
#Oncol#
44
#新诊断#
38
很好的研究
37
厉害
0
#转移性#
36
#转移性前列腺癌#
41
#局部#
34
#局部治疗#
48
#根治#
42