经皮冠状动脉介入治疗(PCI),是指经心导管技术疏通狭窄甚至闭塞的冠状动脉管腔,从而改善心肌的血流灌注的治疗方法。是最为常见的血管成形术,目前可以用于心肌梗死、心脏病和冠心病等。主要的适用范围为慢性稳定型冠心病有较大范围心肌缺血证据的患者,可有效缓解症状。
PCI在世界已经应用有30年历史。最早在1977年由一位瑞士苏黎世医生安德里亚斯·格伦登希所创的,至1980年代全面普及,并广受全球医学界欢迎。主要是通过一根小管,沿动脉通往心脏,在冠状动脉内植入支架,开通闭塞的血管,改善其狭窄的情况。

糖化血红蛋白(GHb)是红细胞中的血红蛋白与血清中的糖类相结合的产物。GHb可有效地反映糖尿病患者过去8~12周平均血糖水平。GHb由HbA1a、HbA1b、HbA1c组成,其中HbA1c约占70%,且结构稳定,因此被用作糖尿病控制的监测指标。
糖尿病与心血管事件风险和心脏介入治疗后的死亡率增加有关。有关心血管疾病背景下最佳血糖控制和HbA1c的文献不断发展。此前已经研究了血糖控制与心脏干预治疗的关系;然而,在这些人群中,并没有持续地证明不良反应与高强度血糖控制的关系。
2000年以前,使用磺脲类药物、比胍类药物和胰岛素控制血糖或HbA1c主要是在 "越低越好 "的口号指导下进行的,但数据参差不齐。为此,最近由美国西奈山大学心脏病学的专家发表在《美国心脏病学会杂志》的研究,评估了一个大型当代队列中PCI术后结局与术前糖化血红蛋白(HbA1c)水平的关系。
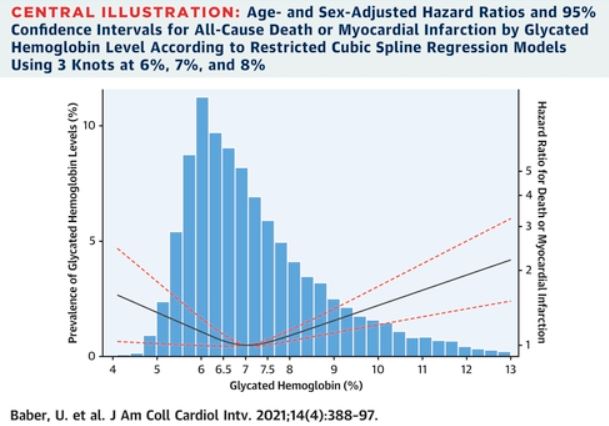
研究人员纳入2009年-2017年在单一机构接受PCI手术的所有已知HbA1c水平的患者。根据HbA1c水平将患者分为5组:≤5.5%、5.6%~6.0%、6.1%~7.0%、7.1%~8.0%和>8.0%。主要终点为PCI术后随访1年的主要心脏不良事件(MACE),即全因死亡或心肌梗死(MI)的综合指标。
共纳入13543名患者(HbA1c≤5.5%,n = 1214;HbA1c 5.6%~6.0%,n = 2202;HbA1c 6.1%~7.0%,n = 4130;HbA1c 7.1%~8.0%,n = 2609;HbA1c >8.0%,n = 3388)。与6.1%~7.0%之间的患者相比,低(HbA1c≤5.5%)和高(HbA1c>8.0%)水平的患者均显示出MACE风险增加。超额风险主要是由低HbA1c水平的人群中较高的全因死亡率所驱动,而较高的数值与较高的MI风险密切相关。
为此,在相关的专家述评中,Harpreet S. Bhatia教授指出,HbA1c较低的患者可能有较差的营养状况和虚弱,导致PCI后死亡风险增加。同时,高肾上腺素能状态和低钾血症导致的心律失常风险潜在增加。此外,葡萄糖变异性与氧化应激和血管炎症的增加有关,以及糖尿病死亡率和血管并发症的增加。
综上,对接受PCI的患者,术前HbA1c水平与1年MACE风险呈现U型关系,这一模式反映了低HbA1c(≤5.5%)的死亡风险更大,而高值(>8.0%)的MI风险更高。因此,HbA1c "越低越好 "的口号或许需要进行更新。
参考文献:
Hemoglobin A1c and Cardiovascular Outcomes Following Percutaneous Coronary Intervention: Insights From a Large Single-Center Registry. J Am Coll Cardiol Cardiovasc Interv. 2021 Feb, 14 (4) 388–397
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#PCI术#
31
#随访结果#
30
#JACC#
27
学习了
53
#ACC#
17
#术后随访#
31
#PCI术后#
36
糖化血红蛋白越低越好
55
还是那个对勾曲线
59
( ˃̶̤́ ꒳ ˂̶̤̀ )
69