ASCO2022:机会之窗临床实验,胶质母细胞瘤的曙光
2022-06-06 影像小生 MedSci原创
神经胶质瘤,尤其是胶质母细胞瘤,今天仍然和20多年前一样令人沮丧。今天的标准治疗方式在很大程度上与过去相同。最重要的进展是在生物学和亚分类上,而不是在治疗上。
2022年ASCO大会于今年6月4日至8日召开,作为全球肿瘤领域最前沿会议,2022年ASCO大会为大家带来了高质量的世界肿瘤治疗的重要研究成果。 今天为大家带来第二日有关胶质母细胞瘤目前研究现状方面内容报道:
今天为大家带来第二日有关胶质母细胞瘤目前研究现状方面内容报道:
神经胶质瘤,尤其是胶质母细胞瘤,今天仍然和20多年前一样令人沮丧。今天的标准治疗方式在很大程度上与过去相同。在过去的20年里,唯一被批准的治疗复发性GBM的药物不能延长生存期。最重要的进展是在生物学和亚分类上,而不是在治疗上。ASCO2022大会汇总了目前胶质母细胞瘤的研究现状。
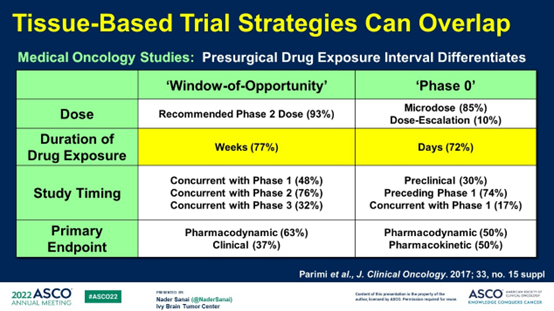
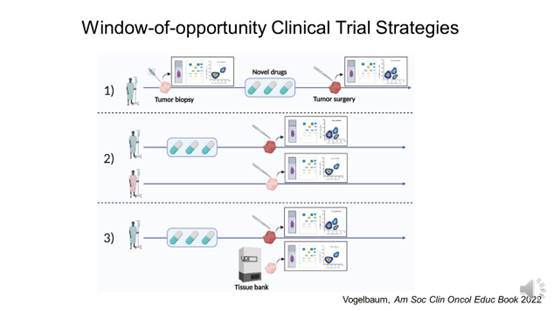
1.RAN0-0期/机会之窗
在25年以上的时间里,只有22个药物试验包括基于组织的药物水平或生物影响分析(血、脑脊液、肿瘤组织、肿瘤侵及大脑)。只有50%的人使用了研究药物的全临床剂量。来自非强化肿瘤的组织样本只分析了大约25%。评估的药物水平约为75%;但是只有68%有生物效应。虽然一些研究声称有效的组织渗透或生物效应,但分析中明显缺失的部分。这些说法在Il或III期研究中都不成立。


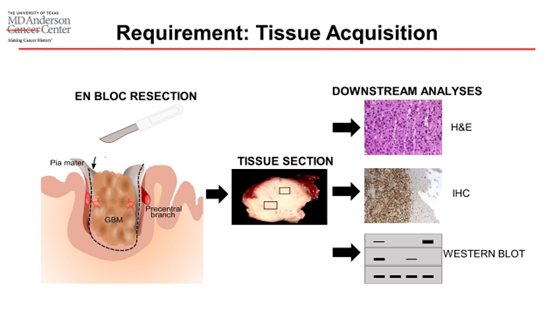
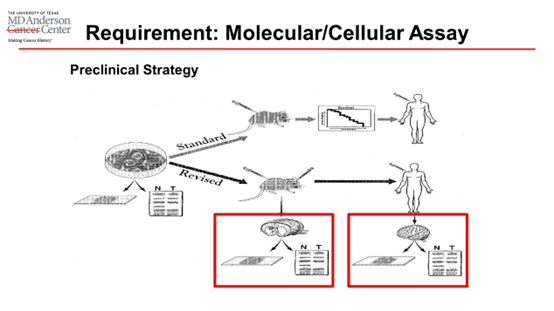
从失败中吸取教训的失败是困扰神经肿瘤学的问题。O期/机会之窗试验为我们提供了一个机会,让我们更好地了解我们的新疗法对患者(而不是小鼠)的生物学效应,以及它们是否有机会发挥作用。我们必须从肿瘤浸润的大脑中提取组织样本,这通常是没有完全切除的。这些设计可以应用于药物(Sanai)、免疫疗法(Heimberger)和工程生物疗法(Lang)的评估。
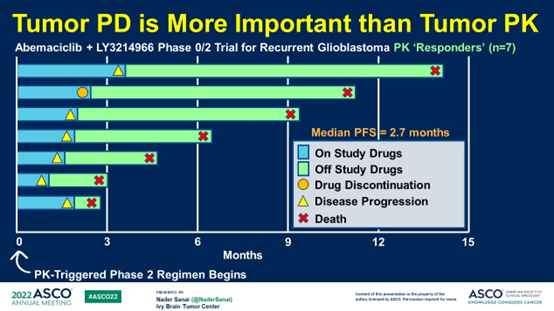
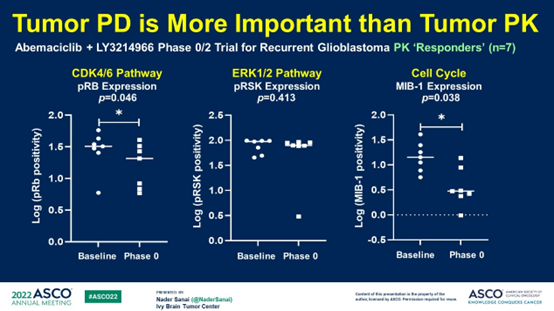
2.胶质母细胞瘤的药代动力学和药效学驱动的临床试验
肿瘤药代动力学比肿瘤药效学更重要。
1) 在更多项目中增加0期和WoO试验
年轻的神经外科医生、神经肿瘤学家、放射肿瘤学家、生物统计学家和神经肿瘤学护士必须接受培训。
2) 加强纵向组织监测
< 15%的试验患者会再次切除。
密集的组织取样可以鉴定对新病原体的遗传适应性。
3) 改进药物传递策略
新技术正在出现,但它们对药物传递的真正影响应该通过PK/PD驱动的研究来量化。

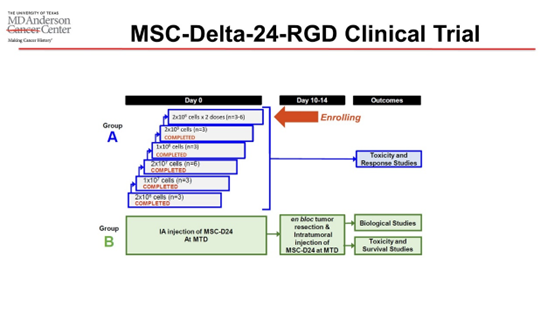
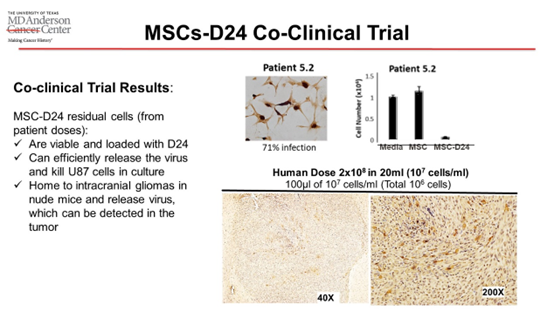
3.机会之窗临床试验:溶瘤病毒治疗的影响
机会之窗试验提供了治疗对人类患者实际肿瘤影响的重要信息,这可能是早期试验最重要的终点。建议大多数早期临床试验纳入机会之窗试验来评估药物对肿瘤的影响。联合临床试验增加了对制剂的保证。机会之窗方法对溶瘤病毒的发展产生了影响。当然机会之窗实验也存在不足:肿瘤切除后,疗效难以评估;手术干预增加了病人的风险;增加成本;收益可能会变慢。
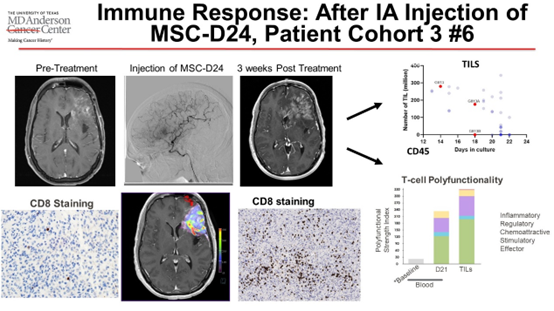

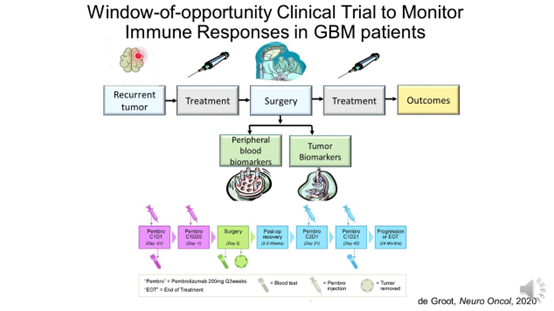
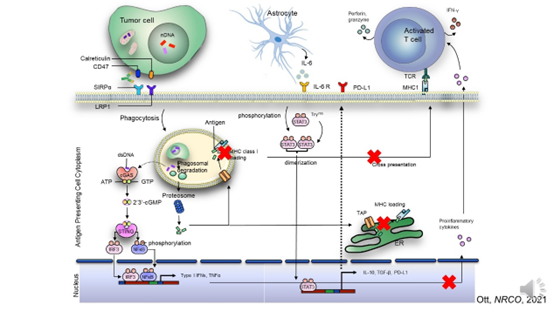
4.通过机会窗临床试验探讨胶质母细胞瘤肿瘤免疫微环境
机会之窗研究可以探究肿瘤微环境的各种类型和效应免疫反应的存在、确定分布,并评估免疫细胞的相互作用(例如,相互作用组)。
局限性:1)纵向评估并非适用于所有类型的恶性肿瘤;2)需要定义最佳监控窗口;3)窗口期可能与药物效应反应不一致。
考虑对肿瘤和邻近的大脑进行取样。
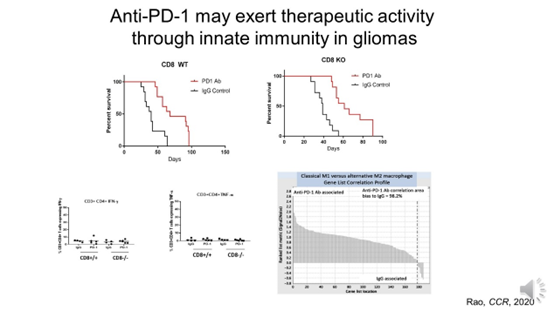
免疫疗法可能不像我们认为的那样起作用:反应的生物标记物可能需要关注先天免疫。
免疫细胞相互作用的探究将越来越多地获得治疗终点和生物标志物的相关性。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ASC#
34
#母细胞瘤#
44
#曙光#
53
#临床实验#
42
#胶质母细胞#
38
#细胞瘤#
39