Neurology:新型tPA替奈普酶用于大动脉闭塞卒中患者更加安全有效!
2022-03-28 网络 网络
替奈普酶(TNK)是一种改良的新型组织纤维溶酶原活化剂(tPA)。
替奈普酶(TNK)是一种改良的新型组织纤维溶酶原活化剂(tPA)。与阿替普酶相比,它具有许多优势,包括更长的半衰期、更高的纤维蛋白特异性和更低的纤维蛋白原耗竭可能性。与阿替普酶相比,治疗急性缺血性卒中的疗效和安全性提高的潜力已经推动了几项正在进行的临床试验。
最近建议根据对选定的血栓切除术前患者的疗效和一项新的非劣效性荟萃分析来改变常规实践以支持未经许可使用替奈普酶然而,由于易于给药——阿替普酶单次推注而不是推注后 1 小时输注——这在医院之间患者转移的情况下尤其有利。
目前,对80岁以上患者使用TNK的详细研究是有限的。为了评估TNK在80岁以上大血管闭塞患者中0.25和0.40mg/kg剂量的安全性和有效性,来自澳大利亚墨尔本脑科中心的医学和神经科的专家开展了相关研究,结果发表在Neurology杂志上。

研究人员对EXTEND-IA TNK随机对照试验进行了汇总分析(n = 502)。患者是在症状发生后4.5小时内出现的因颅内颈动脉、大脑中动脉或基底动脉闭塞导致的缺血性卒中的成年人。主要比较了TNK 0.25mg/kg、TNK 0.40mg/kg和阿替普酶0.90mg/kg的治疗效果,对患者年龄(>80岁)进行分层。评估的结果包括90天改良的Rankin量表(mRS)评分、全因死亡率和有症状的ICH。
结果显示,在大于80岁的患者中(n = 137),TNK 0.25 mg/kg与0.40 mg/kg相比,90天mRS得到改善(中位数3 vs 4,acOR=2.70,95% CI 1.23-5.94),死亡率降低(acOR=0.34,95% CI 0.13-0.91)。TNK 0.25 mg/kg与阿替普酶相比,90天mRS改善(中位数3 vs 4,acOR= 2.28,95% CI 1.03-5.05)。
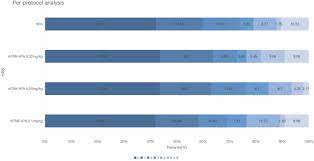
阿替普酶和TNK 0.40 mg/kg之间没有发现90天mRS或死亡率的差异。4名接受TNK 0.40 mg/kg治疗的患者出现症状性ICH,1名接受阿替普酶治疗的患者,以及0名接受TNK 0.25 mg/kg治疗的患者。在≤80岁的患者中,TNK 0.25 mg/kg、阿替普酶和TNK 0.40 mg/kg的90天mRS、死亡率或症状性ICH均无差异。
综上,TNK 0.25 mg/kg与80岁以上患者90天mRS的改善和死亡率的降低有关。在年轻患者中没有观察到不同剂量的差异。
参考文献:
Safety and Efficacy of Tenecteplase in Older Patients With Large Vessel Occlusion A Pooled Analysis of the EXTEND-IA TNK Trials. Neurology Mar 2022, 98 (12) e1292-e1301; DOI: 10.1212/WNL.0000000000013302
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#卒中患者#
48
#tPA#
33
#大动脉闭塞#
48
#动脉闭塞#
42
#Neurol#
34
#替奈普酶#
55