JPD:帕金森患者,长期的认知和运动障碍变化规律有何特点?
2022-03-20 freeman爱科学 MedSci原创
在三年的时间里,不同的PD运动表型有不同的神经心理学进展模式。
人们越来越努力地确定帕金森病(PD)中认知能力下降和发生痴呆的潜在风险因素。大约30-40%的帕金森病患者存在认知障碍,患病率在病程中不断增加,10年后可达50%,在诊断后20年达到80%。
与帕金森病相关的认知状况是异质性的。由于已知的前纹状体功能障碍,执行功能以及注意力和工作记忆方面的缺陷经常出现在PD的早期阶段。PD晚期的痴呆症发病率很高,约为50%,其认知状况通常与记忆和视觉空间能力的额外缺陷有关,这被认为是晚期颞顶功能障碍的反映。
患者可分为震颤主导型(TR-D)、姿势不稳步态障碍(PIGD)或未确定(ND)运动表型。还有人将患者分为震颤主导型、运动迟缓型和混合型表型。一些可改变的因素与PD的认知损害有关,我们以前曾表明,不同的认知特征与不同的运动表型有关。我们对LANDSCAPE队列的横断面报告,这是一项调查PD患者认知功能的多中心纵向观察研究,描述了TR-D患者的认知缺陷似乎不那么严重,而PIGD患者在执行功能方面表现较差,这又与非震颤运动评分呈负相关。
同样,运动表型也可能影响认知障碍的进展,因为有证据表明,PIGD患者不仅表现出更快的认知衰退,而且有更大的痴呆风险和更高的抑郁率。这可能与运动表型的作用和认知障碍的进展特别相关,因为最初表现为TR-D患者的病人往往在病程中转换为PIGD型。
藉此, 德国RWTH Aachen University Hospital的Jennifer Michels 利用DEMPARK/LANDSCAPE研究的长期数据,评估认知障碍的进展和运动表型对PD认知衰退的预测价值。
他们纳入了711名PD患者的人口统计学、临床和神经心理学六年的纵向数据(年龄:M = 67.57;67.4%为男性)。并计算了认知领域的Z转换综合得分。对年龄、性别、教育和疾病持续时间进行了分析控制。
为了尽量减少数据缺失和辍学,他们使用线性混合模型评估了442名PD患者的三年随访数据,以了解运动表型对认知能力下降的具体作用(年龄:M=66.10;68.6%的男性)。
他们发现:在疾病的过程中,运动症状增加,而MMSE和PANDA在所有亚组中保持稳定。
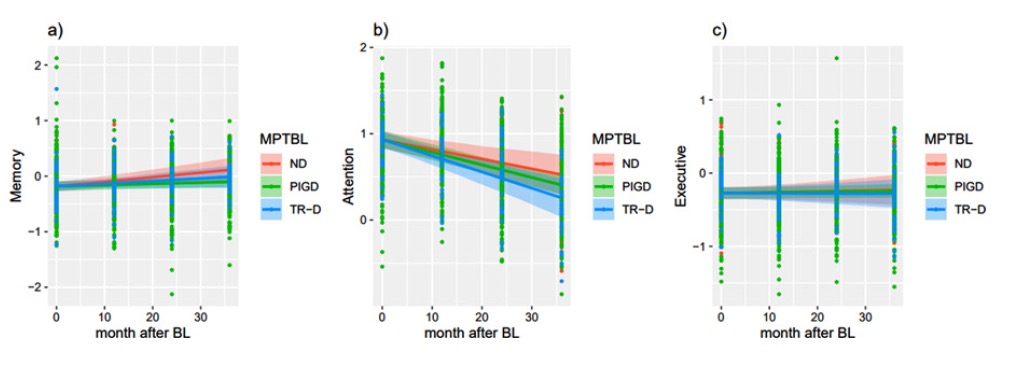
经过三年的随访,PIGD患者的整体认知能力明显下降,运动表型在注意力(β=-0.08,SE=0.003,p<0.006)和记忆功能方面存在差异,显示PIGD患者与ND组相比,每个月恶化-0.006(SE = 0.003,p = 0.046)。
此外,PIGD患者在日常生活中更经常遇到困难。
该研究的重要意义在于发现了:在三年的时间里,不同的PD运动表型有不同的神经心理学进展模式,早期的执行缺陷在后期的过程中产生了更多的失忆特征。特别是PIGD患者与TR-D和ND患者相比,随着时间的推移而恶化,突出表明这种运动表型的痴呆风险更大。
原文出处:
Michels J, Storch A, Linse K, et al. Long-Term Cognitive Decline Related to the Motor Phenotype in Parkinson’s Disease.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















写的很好
47
学习了
59
#运动障碍#
47
学习了
58
不错,学习了。
66
受益匪浅
54