Mol Cancer Ther:MDA-9/Syntenin (SDCBP) PDZ1小分子抑制剂能够抑制前列腺癌发病机制
2019-08-12 AlexYang MedSci原创
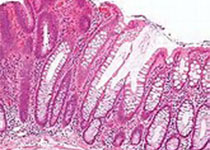
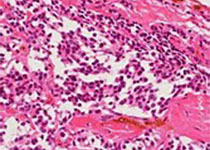
转移是许多实体肿瘤导致患者死亡的主要决定性因素,并且MDA-9/Syntenin (SDCBP),一个促进转移和促进血管生成基因能够促进上述结果。之前,有研究人员阐述了MDA-9/Syntenin能够通过与IGF-1R物理互作,激活STAT3并调控前列腺癌的发病机理。这些结果强烈的支持了MDA-9可以作为前列腺癌的一个潜在分子靶标。MDA-9/Syntenin包括了2个高度同源PDZ结构域,并预测
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#MDA#
38
#CBP#
27
#抑制剂#
30
#小分子#
27
#DCB#
39
#小分子抑制剂#
30
#癌发病#
19
前列腺癌相关研究,学习了,谢谢梅斯
50