JAHA:升主动脉长度与A型主动脉夹层的关系
2021-06-14 MedSci原创 MedSci原创
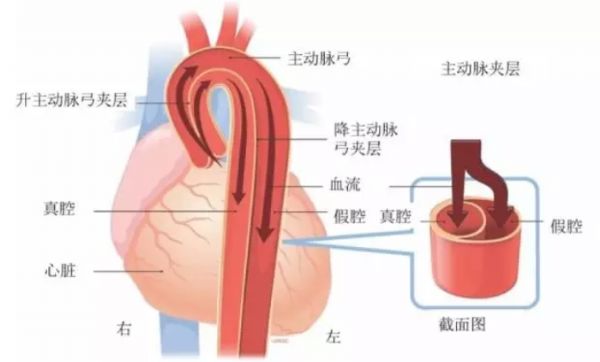
在调整年龄、性别和主动脉直径后,升主动脉的长度可能有助于鉴别A型夹层患者、正常对照组和非夹层胸动脉瘤患者。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在明确升主动脉长度和直径在A型主动脉夹层中的意义。

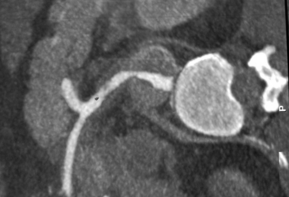
研究人员对51例急性A型动脉瘤患者、121例近段胸主动脉瘤患者和200例正常主动脉对照者的进行CT扫描,并通过多平面重建对主动脉环到无名动脉这一节段进行分析。
在对照组中,升主动脉长度与直径(r2=0.35, P<0.001)、年龄(r2=0.17, P<0.001)、性别(P<0.001)相关。由于主动脉在急性夹层时形态发生了直接变化,研究人员根据已发表文献中的模型估算了夹层前的长度和直径。急性夹层患者(中位数为109.7mm;四分位数范围[IQR]为101.0-115.1 mm)、估计的夹层前患者(中位数为104.2mm;IQR为96.0-109.3 mm)、动脉瘤患者(中位数为107.0 mm;IQR为99.6-118.7 mm)升主动脉长度较长,相比于对照组(中位数为83.2mm;IQR为74.5-90.7mm)(所有比较P<0.001)。

动脉瘤患者升主动脉直径最大(中位数为52.0mm;IQR为45.9-58.0mm),其次是夹层患者(中位数为50.3mm;IQR为46.6-57.5 mm),而对照组和估计的夹层前患者组之间没有显著差异(中位数为33.4 mm [IQR为30.7-36.7 mm]和35.2mm [IQR为32.6-40.3 mm], P=0.09)。调整直径、年龄和性别调整后,估计的夹层前患者主动脉长度比对照组长16mm,比非夹层胸动脉瘤患者长12mm。
由此可见,在调整年龄、性别和主动脉直径后,升主动脉的长度可能有助于鉴别A型夹层患者、正常对照组和非夹层胸动脉瘤患者。
原始出处:
Daniella Eliathamby.et al.Ascending Aortic Length and Its Association With Type A Aortic Dissection.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/10.1161/JAHA.120.020140
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#A型主动脉夹层#
44
#AHA#
41
#主动脉#
47
#动脉夹层#
54
佩服
73
👍
75
好人一生平安
82