Acta Neuropathologica: 幕下C11orf95融合胶质瘤与幕上RELA融合室管膜瘤共有组织学、免疫表型和分子特征
2020-11-25 MedSci原创 MedSci原创
室管膜瘤是一组异质性胶质瘤,它发生在中枢神经系统的不同部位,表现出广泛的组织病理学特征。DNA甲基组分析和转录组分析已经确定了至少9个由解剖位置和分子改变分开的室管膜瘤分子群。
室管膜瘤是一组异质性胶质瘤,它发生在中枢神经系统的不同部位,表现出广泛的组织病理学特征。DNA甲基组分析和转录组分析已经确定了至少9个由解剖位置和分子改变分开的室管膜瘤分子群。幕上室管膜瘤的特点是包含RELA或YAP1的基因融合。后颅窝(PF)室管膜瘤有两大类:PFA发生在预后较差的幼儿,而PFB发生于年龄较大的儿童和成人,预后较好。目前已经观察到有C11orf95 RELA融合的PF室管膜瘤,尽管它们位于幕下,但仍不清楚它们是否代表室管膜瘤的一个明显的亚型,还是与ST RELA融合的室管膜瘤密切相关。
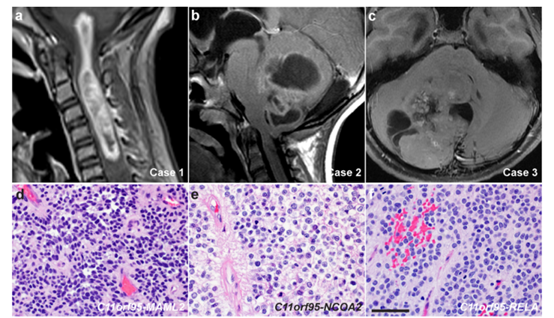
本文发现了三个幕下胶质瘤(一个颈髓部和两个小脑)的组织病理学特征与ST-RELA融合室管膜瘤非常相似:所有肿瘤均为非浸润性生长,边缘与邻近小脑或脊髓组织不同。同一肿瘤的细胞学和结构各不相同,但单一的肿瘤细胞群、细胞质清晰、血管周围无环带和营养不良的微钙化是一致的特征。颈髓肿瘤还表现为局灶性乳头状生长。有丝分裂活性是显而易见的,并且Ki-67标记在所有肿瘤中都很高,证明了高级别的标记。所有肿瘤均表现为ST-RELA融合室管膜瘤的特征性免疫表型--存在可变的GFAP免疫反应。Olig2和Sox10偶尔在细胞中表达。所有肿瘤中L1CAM呈弥漫性强阳性,组蛋白H3 K27残基三甲基化保留核免疫反应性。
方法:荧光原位杂交(FISH)分别在2例(病例2和3)和1例(病例3)肿瘤中识别出C11orf95和RELA的重排。通过RNA序列分析,我们在这些肿瘤中发现了C11orf95-MAML2、C11orf95-NCOA2和C11orf95相关融合。在ST室管膜瘤中发现了C11orf95-MAML2和C11orf95相关融合,而C11orf95-NCOA2融合是一个新发现。除病例3的等位基因频率为8%的BCOR V406fs亚克隆变体外,所有肿瘤的per外显子测序均为阴性。FISH未发现染色体臂1q的增加、PFA和PFB的不良预后因子以及CDKN2A/B的缺失。
结论:研究表明,RELA融合的室管膜瘤不需要涉及RELA的融合转录本来产生病理组织学和分子标记。本文的发现拓宽了C11orf95融合室管膜瘤的范围,并对室管膜肿瘤的诊断和分类有指导意义。
Keenan, C., Graham, R.T., Harreld, J.H. et al. Infratentorial C11orf95-fused gliomas share histologic, immunophenotypic, and molecular characteristics of supratentorial RELA-fused ependymoma. Acta Neuropathol 140, 963–965 (2020). https://doi.org/10.1007/s00401-020-02238-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#组织学#
40
#管膜瘤#
63
#CTA#
37
#Pathol#
38
#分子特征#
35
#pathologic#
29
#融合#
23
#表型#
27
#室管膜瘤#
39
#室管膜瘤#
29