Eur Heart J:房颤患者慢性阻塞性肺疾病的患病率、治疗和影响
2021-08-02 MedSci原创 MedSci原创
COPD在AF患者中很常见,13%的AF患者伴有COPD,并且与合并症负担增加、差异化管理和更差的结局相关,全因死亡风险增加两倍以上,此外大出血和心血管死亡风险增加。
房颤(AF)患者慢性阻塞性肺疾病(COPD)的患病率尚未明确,并且其与不良结局之间的关联经常被忽视。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在评估COPD的患病率、其对AF患者临床管理和结局的影响,以及β受体阻滞剂(BBs)对COPD患者结局的影响。
研究人员根据国际准则进行了系统评价和荟萃分析,纳入了所有报告AF患者COPD患病率的研究。根据COPD和BB使用状态比较了合并症、BBs和口服抗凝剂处方以及结局(全因死亡、心血管(CV)死亡、缺血性卒中、大出血)的数据。
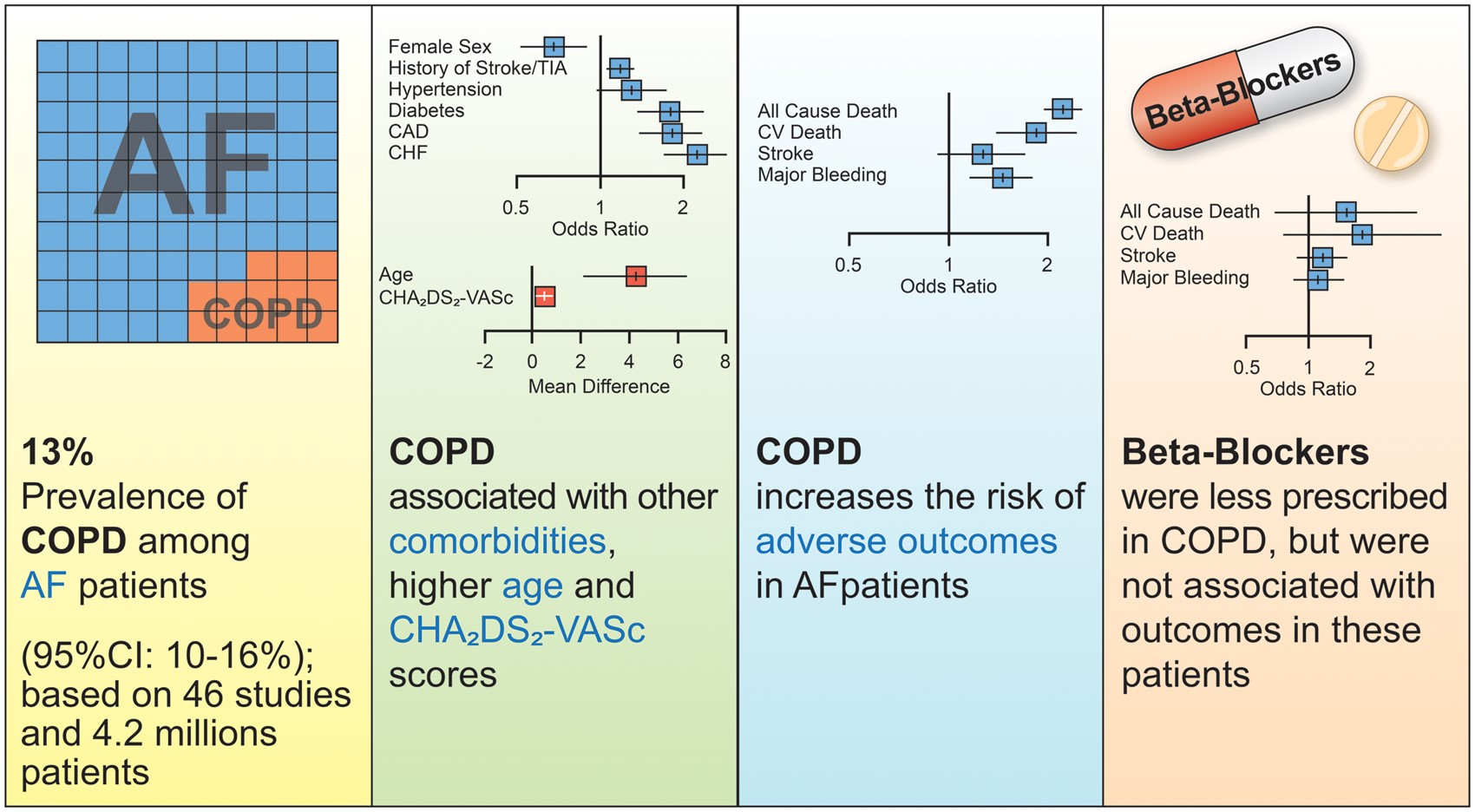
在46项研究中,COPD的合并患病率为13%[95%置信区间(CI)为10-16%,95%预测区间为2-47%]。COPD与较高的合并症患病率、较高的CHA2DS2-VASc评分和较低的BB处方相关[比值比(OR)为0.77,95%CI为0.61–0.98]。COPD与全因死亡(OR为2.22,95%CI为1.93-2.55)、心血管死亡(OR为1.84,95%CI为1.39-2.43)和大出血(OR为1.45,95%CI为1.17-1.80)风险相关。
COPD在AF患者中很常见,13%的AF患者伴有COPD,并且与合并症负担增加、差异化管理和更差的结局相关,全因死亡风险增加两倍以上,此外大出血和心血管死亡风险增加。BBs治疗不会增加伴有COPD的AF患者不良结局的风险。
原始出处:
Giulio Francesco Romiti.et al.Prevalence, management and impact of chronic obstructive pulmonary disease in atrial fibrillation: a systematic review and meta-analysis of 4,200,000 patients.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab453
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阻塞#
0
学习了,谢谢啦
79
#患病率#
36
#ART#
41
#HEART#
37
#房颤患者#
30
#房颤#患者#慢性阻塞性肺疾病#
140
房颤,临床上碰到很多哦
69