单孔机器人辅助肾移植和自体肾移植的初步经验
2021-09-05 泌尿小王 MedSci原创
单端口机器人入路用于肾移植(KT)具有进一步降低KT发病率的潜力。
与标准的开放方法相比,多端口机器人辅助肾脏移植(RAKT)已经成为一种新的替代方法。近年来,RAKT已成为传统开放技术的一种微创替代品。寻求微创肾移植方法的最初动机与开放手术伤口相关并发症的显著高发生率有关,特别是患者处于免疫抑制和/或身体肥胖的状态下。单端口机器人入路用于KT是否具有进一步降低KT并发症的潜力依然未知。
《欧洲外科杂志》近日发表了一篇单孔机器人RAKT的研究,结果显示单端口RAKT是可行的而且安全有效,具有潜在的好处。
方法
研究对象
来自活着或死去的供者的同种异体肾移植到6名终末期肾病患者体内。单孔机器人手术通过5厘米中线脐周腹部切口经腹膜或腹膜外入路形成。采用相似的切口和技术,对3例患者进行了右或左肾切除和自体移植手术。
排除标准是:年龄小于18岁的患者、机器人手术的任何禁忌症、需要不止一次动脉吻合的复杂血管移植物解剖和需要自体肾切除术的患者。
在所有的受者中,术前非造影计算机断层扫描评估髂外动脉的解剖和结构(动脉粥样硬化斑块)。
我们选择脑死亡供体,肾脏供体指数(>50%)高,主动脉斑块最少(如果有的话),没有其他大体解剖异常。
手术方式
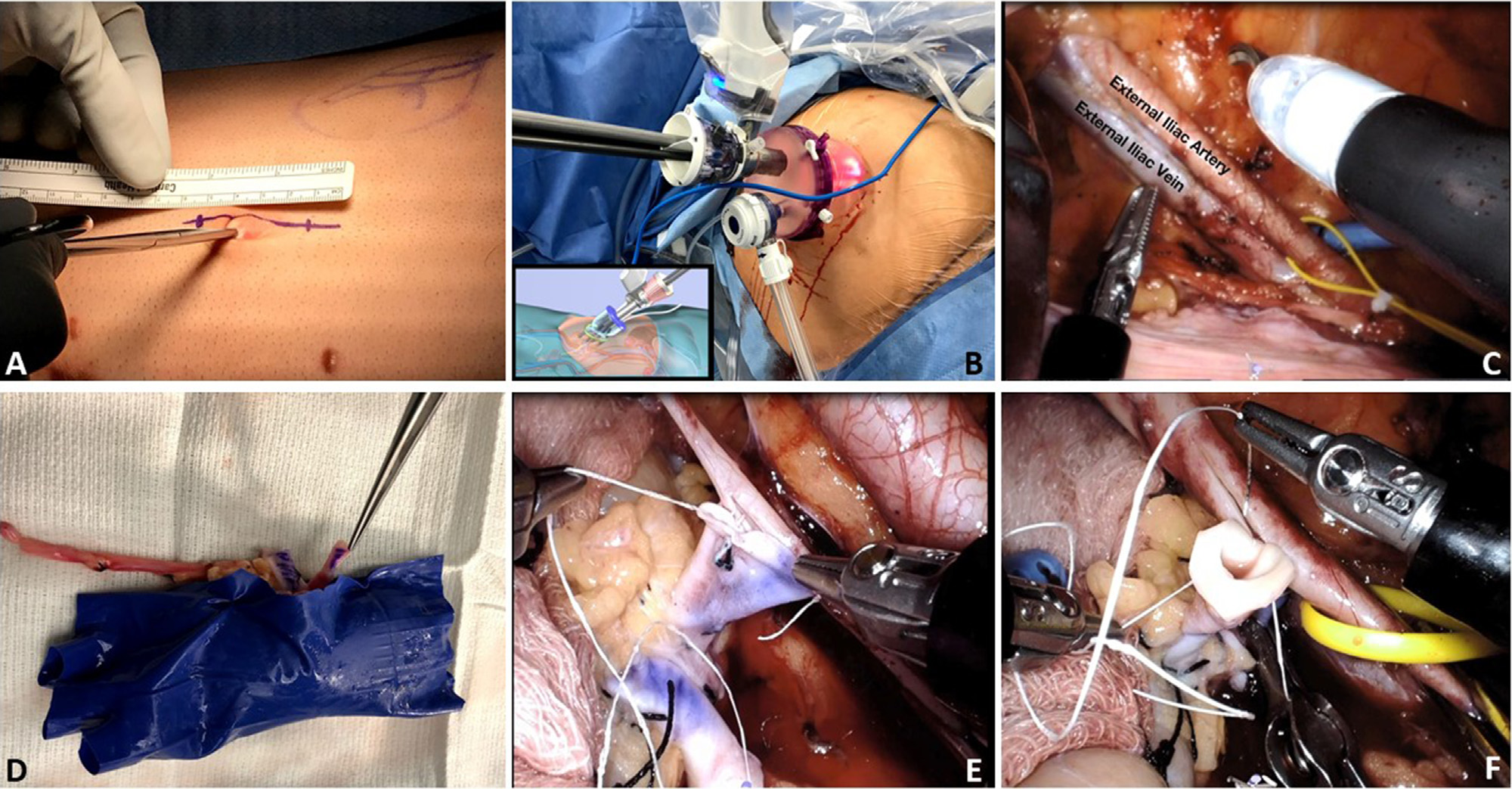
(A)单孔机器人辅助肾移植从脐周5cm切口开始。
(B)然后,单口机器人通过GelPOINT系统对接。
(C)解剖髂外静脉、动脉,准备血管吻合。
(D)肾套叠后,将移植物包裹在外科手套内作为外套,用记号笔标记肾动静脉后表面。
将移植物置于腹部进行
(E)静脉吻合
(F)动脉吻合
结果
单端口RAKT手术成功完成,全手术和血管吻合时间分别为300 - 450分钟和52 - 92分钟。最后一次随访时间(2周到1年),所有6例患者的移植肾功能良好,血清肌酐水平从1.2到1.5 mg/dl分布不等。在3例患者中,用单端口机器人入路成功地完成了自体肾移植。
手术和血管吻合总时间分别为510 ~ 600分钟和65 ~ 83分钟。在这三例患者中,术后和随访中血清肌酐水平均保持正常,在撰写本文时(手术后4-8个月)均无症状。
结论
在这一初步经验中,证明了该技术的安全性和可行性,具有良好的早期移植物功能。虽然这些早期结果很有希望,但还需要更大规模的随访。如果未来的比较试验证实,进一步降低KT发病率可能与改善康复有关,减少并发症、住院和术后疼痛。
文献来源:Kaouk J, Eltemamy M, Aminsharifi A, et al. Initial Experience with Single-port Robotic-assisted Kidney Transplantation and Autotransplantation. Eur Urol. 2021 Sep;80(3):366-373. doi: 10.1016/j.eururo.2021.03.002. Epub 2021 Mar 31. PMID: 33810922.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#机器人#
31
#机器人辅助#
0
#机器#
38
受教
49
学习学习
0