NEJM:白细胞介素-33单抗Itepekimab可降低重度哮喘患者哮喘病情失控风险
2021-11-01 MedSci原创 MedSci原创
通过抑制白细胞介素-33,Itepekimab降低了中重度哮喘患者哮喘病情失控风险,改善患者肺功能及生活质量

哮喘不是一种简单的疾病,具有许多表型和内型,大致可分为2型哮喘或非2型哮喘,临床上常见的2型哮喘有早期过敏性哮喘、晚期嗜酸性哮喘或运动性哮喘。目前严重2型哮喘的治疗靶点主要包括IgE、白细胞介素-4、白细胞介素-13以及白细胞介素-5。全基因组关联研究表明,白细胞介素-33与哮喘易感性之间存在遗传关联。近日研究人员考察了白细胞介素-33单抗Itepekimab治疗严重哮喘的效果。

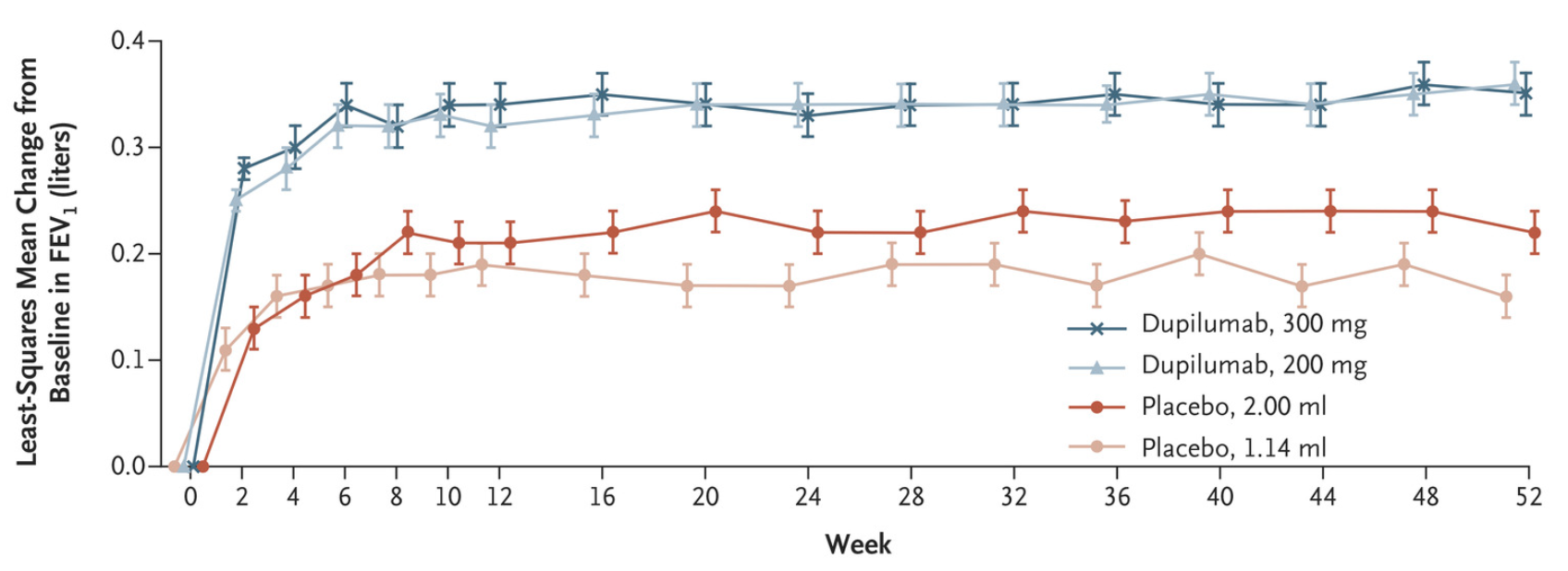
本次研究为II期临床研究,重度哮喘患者在接受吸入糖皮质激素联合长效β-激动剂(LABA)治疗基础上,随机接受皮下注射Itepekimab(剂量为300 mg)、Intpekimab+ Dupilumab(均为300 mg;联合治疗组)、Dupilumab(300 mg)或安慰剂,每2周一次,持续12周。分组后,LABA在第4周停止,吸入糖皮质激素在第6至9周逐渐减少。研究的主要终点为Itepekimab治疗后哮喘病情失控,次要终点和其他终点包括肺功能、哮喘控制、生活质量、2型生物标志物和安全性。
总计296名患者参与研究。到12周时,Itepekimab组22%的患者、Intpekimab+ Dupilumab联合治疗组27%的患者以及Dupilumab组19%的患者哮喘病情失控,而安慰剂组为41%。与安慰剂相比,Itepekimab、Intpekimab+ Dupilumab以及Dupilumab组哮喘病情失控的风险分别为0.42、0.52和0.33。与安慰剂相比,Itepekimab和Dupilumab单药治疗组在使用支气管扩张剂前1秒用力呼气量增加,而联合治疗组则没有增加。与安慰剂相比,Itepekimab治疗改善了哮喘控制和生活质量,并导致平均血嗜酸性粒细胞计数显著降低。组间不良事件发生率相似。
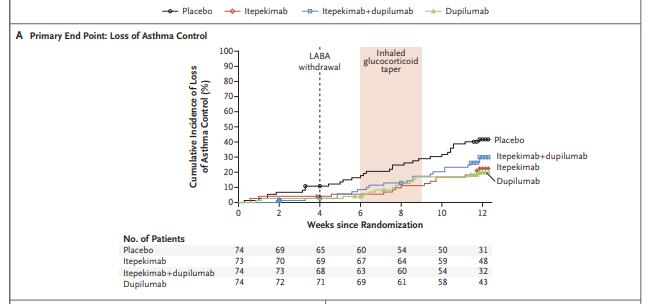
组间哮喘控制率
研究发现,通过抑制白细胞介素-33,Itepekimab降低了中重度哮喘患者哮喘病情失控风险,改善患者肺功能及生活质量。
原始出处:
Michael E. Wechsler. Efficacy and Safety of Itepekimab in Patients with Moderate-to-Severe Asthma. N Engl J Med,October 28,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#重度哮喘#
35
#PE#
32
#病情#
26
#mAb#
38
#白细胞介素#
51
学习学习学习
79
学习
86