medRxiv:暨南大学周庆华研究员参与的队列研究,揭示全外显子组测序在妊娠流产中的临床实用性
2020-07-30 转化医学网 转化医学网
众所周知,基因异常会导致妊娠丢失。最近的WES研究在84例有超声异常的胎儿死亡病例中分别检测到阳性、可能和候选变异的20%、45%和9%,在19例错失流产的POC病例中,有15例存在序列变异。在一个由
众所周知,基因异常会导致妊娠丢失。最近的WES研究在84例有超声异常的胎儿死亡病例中分别检测到阳性、可能和候选变异的20%、45%和9%,在19例错失流产的POC病例中,有15例存在序列变异。在一个由70个与心脏通道病变和心肌病相关的基因组成的小组中,有12%的死产患者检测到致病性变体。尽管病例选择标准不同,且变异分类不一致,但是这些研究,积累的研究数据表明,外显子组测序可能有助于识别相当一部分妊娠损失病例的单基因原因,并应纳入诊断实践。
中国广州暨南大学生物医学转化研究院周庆华研究员,与美国科学家一同在预印本medRxiv上发表了一项研究。这项研究支持了全外显子组测序(WES)在检测妊娠丢失的单基因病因方面的临床实用性,新变体的发现可为引起胎儿死亡的潜在分子机制提供新的见解。
这项研究选择了102例具有正常核型且无致病性拷贝数变异的受孕产物(POC)样本中选择样本进行WES研究,评估异常检测率(ADR)以及与自然流产(SAB)和死胎相关的诊断值变异。
结果表明,WES检测到6种致病性变异体,16种可能致病性变异体,17种不确定意义的变异体有利于致病性(VUSfp)。致病性和可能致病性变体的ADR为22%,加入VUSfp后,ADR为35%。SAB和死胎的不良反应率分别为36%和33%。受影响的基因包括与多系统异常、神经发育障碍、心脏异常、骨骼发育不良、代谢紊乱和肾脏疾病相关的基因。
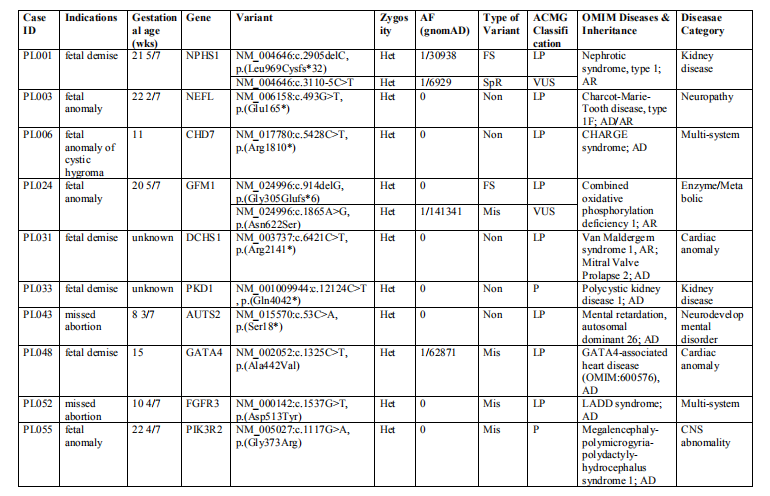
本研究检测到的致病性和可能的致病性变体
这些结果支持WES检测单基因妊娠丢失的临床应用价值。疾病相关变异的鉴定为后续的复发风险遗传咨询和后续妊娠的处理提供了信息。新变异的发现可以为揭示导致胎儿死亡的潜在分子机制提供线索。
不过,这项研究有一些局限性,因此克服这些局限性的方法应在临床应用和进一步研究中加以实施。首先,虽足以验证WES的临床效用,但样本量不足以对妊娠丢失的遗传病因进行全面评估。考虑到这一队列研究和其他研究中显示的疾病类型的异质性,需对11个病例进行协作研究,以研究胎儿死亡的单基因病因。第二,研究使用的样本被取消鉴定,没有进行后续的亲子研究。最后,本研究只关注OMIM基因,而不是用来评估可能对胎儿生长发育很重要的非OMIM基因。此外,使用细胞和动物模型的研究应该是未来研究设计的一个组成部分,以阐明已识别的变异,特别是反复和新的变异对胎儿死亡的功能影响。
总之,这项研究表明22%-35%的妊娠损失在可能导致胎儿死亡的基因中具有诊断价值的变体,这支持了WES作为一种有价值的基因检测工具来识别妊娠损失的原因。识别与胎儿死亡相关的复发基因和变异可能有助于更好地了解已知OMIM基因在胎儿发育中的功能及其在妊娠损失中的作用。诊断价值变异的鉴定为复发风险评估、后续的父母研究、产前基因咨询和后续怀孕的管理提供了必要的信息。
原始出处:
Chen Zhao, Hongyan Chai, Qinghua Zhou, et al. Whole-exome sequencing analysis on products of conception: A cohort study to evaluate clinical utility and genetic etiology for pregnancy loss.medRxiv, 2020, doi: https://doi.org/10.1101/2020.07.19.20150144.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#研究员#
31
#全外显子组测序#
32
#外显子组测序#
34
#外显子组#
55
#实用性#
33
#medRxiv#
36
#Med#
23
#外显子#
33