
临床观察和新出现的研究表明,患有多发性硬化症(MS)的美国黑人(BA)往往比他们的美国白人(WA)同行的情况更糟糕。以前的研究表明,相对于美国白人而言,患有多发性硬化症的BA的疾病负担更重。
研究报告称,与美国白人相比,BAs的残疾积累更多,更早发展到需要流动协助,脑部MRI上的病变积累更快,脑部和视网膜组织损失更快,视神经炎后高对比度视力损失更多。
尽管有这些报道,已发表的研究在知识方面产生了一些差距,部分是由于研究设计和方法的局限性。较大的研究主要是回顾性的,集中在对残疾的全面测量(即扩展的残疾状态量表[EDSS],多发性硬化症严重程度评分[MSSS]),这些半定量的量表主要是评估移动功能。
许多评估其他结果的研究,特别是大脑或视网膜萎缩的研究,BA的样本很小,或者是单中心研究,因此,估计的精确度以及所研究的病人的代表性是令人担忧的。此外,种族与社会经济地位的交集是一个已知的决定健康的有力因素,因为它与多发性硬化症的结果有关,在美国的人群中还没有得到很好的描述。
为了解决之前研究的这些缺陷,霍普金斯大学的Karla Gray-Roncal等人,在美国的BA和WA多发性硬化症患者的大型多中心队列中,全面比较了神经功能和疾病严重程度,并评估种族和社会经济地位与这些措施之间的相互作用。
方法。他们比较了多发性硬化队列(MS PATHS)队列中的BA和WA参与者,在协变量调整(包括教育水平、就业或保险作为社会经济指标)后,MS特征包括自我报告的残疾、客观的神经功能评估和定量的脑MRI测量。在亚组中,他们使用9位数的邮政编码评估了种族内、邻里层面的社会经济地位(SES)指标。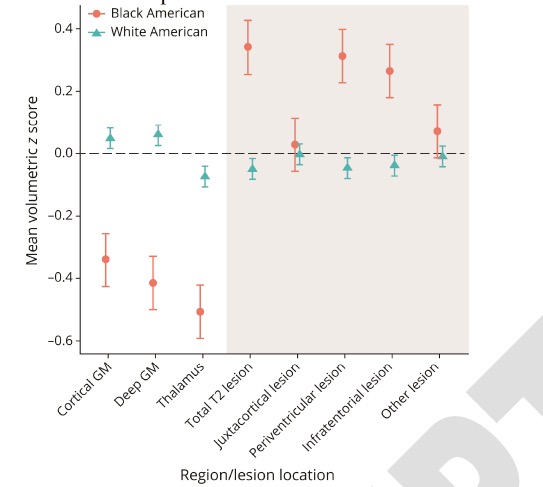
他们发现,在1,214名BA和7,530名WAs患者中,BA更年轻,教育水平更低,比WAs更可能有医疗补助保险或残疾或失业。
BAs自我报告的残疾情况更差(重度残疾与轻度残疾的几率大1.47倍,95% CI 1.18, 1.86),在认知处理速度(正确率降低5.06,CI -5.72, -4.41)、行走(慢0.66秒,95% CI 0.36, 0.96)和手工灵活性(慢2.11秒,95% CI 1.69, 2.54)的测试中表现更糟。
BAs有更多的脑部MRI病变,整体和灰质脑容量较低,包括丘脑(-0.77毫升,95%CI-0.91,-0.64)、皮质(-30.63毫升,95%CI-35.93,-25.33)和深层(-1.58毫升,95%CI-1.92,-1.23)灰质容量减少。
虽然较低的SES与WA中较差的神经表现分数相关,但这种关联在BA中却不太明显。
这个研究的重要意义,在于发现了:相对于WAs的MS,BAs的疾病负担更大。除了SES,未来的纵向研究还应该考虑其他社会结构的作用。这类研究对于确定预后因素和患有多发性硬化症的BAs的最佳治疗策略,意义重大。
原文出处:
Gray-Roncal K, Fitzgerald K, Ryerson LZ, Charvet L, Cassard SD, Naismith R, Ontaneda D, Mahajan K, Castro-Borrero W, Mowry E. Association of Disease Severity and Socioeconomic Status in Black and White Americans With Multiple Sclerosis. Neurology. 2021 Jun 30:10.1212/WNL.0000000000012362. doi: 10.1212/WNL.0000000000012362. Epub ahead of print. PMID: 34193590.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#多发性#
40
#Neurol#
42
学习了
49
学习了
64
生而不同~
63