EClinicalMedicine:合并2型糖尿病和或慢性肾病的心衰患者近20多年的预后变化趋势
2021-02-08 MedSci原创 MedSci原创
心力衰竭(HF)与2型糖尿病(T2D)和慢性肾脏病(CKD)一起是二十世纪的三大主要流行病。
心力衰竭(HF)与2型糖尿病(T2D)和慢性肾脏病(CKD)一起是二十世纪的三大主要流行病。目前还不知道,在过去20年里,在新发HF患者中,T2D和CKD合并症与特定病因住院和死亡之间有哪些独特而综合的关联。
Lawson等人采用英国临床实践研究数据与英格兰医院统计数据(1998-2017年)相链接,开展了一项观察性研究。纳入≥30岁的新发HF患者。分组:(i)HF不合并T2D和CKD(对照组);(ii)HF仅合并CKD(HF-CKD);(iii)HF仅合并T2D(HF-T2D);(iv)HF同时合并T2D和CKD(HF-T2D-CKD)。CKD严重性分组:CKD-3a (eGFR[ml/min·1.73m2] 45–59); CKD-3b (30–44); CKD-4 (15–29); CKD-5 (<15)。预后为心血管和非心血管住院率和全因死亡率。
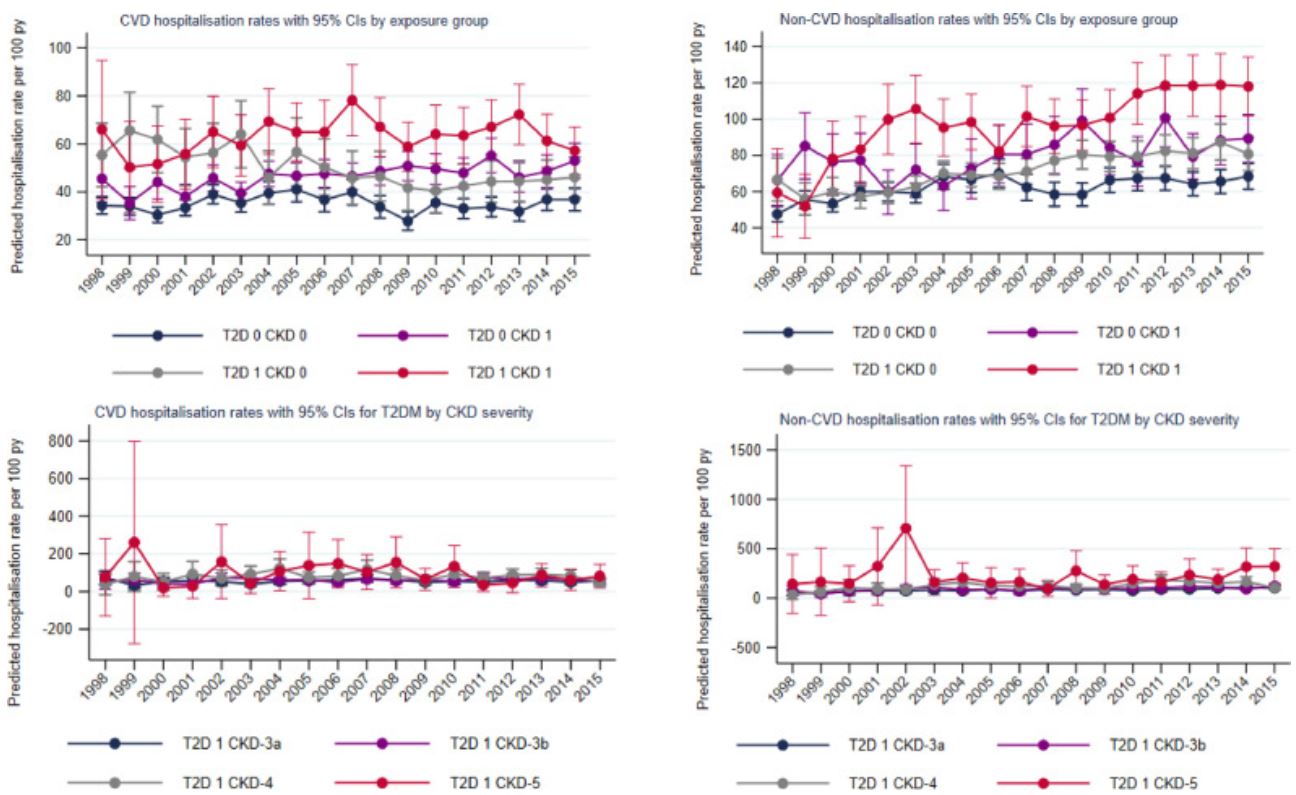
估计1年特异性原因住院率的变化趋势
共纳入了87709位HF患者(平均78岁,49%女性),40%的患者为HF-CKD,12%的患者为HF-T2D,16%的患者为HF-T2D-CKD。与对照组相比,HF-CKD和HF-T2D组的HF患者的年龄标准化的第一年CVD住院率明显更高(46.4和49.2 vs 35.1/100人·年),HF-T2D-CKD组中CKD-5的患者的最高(89.1/100人·年)。非CVD住院率和死亡率也有相似的模式。调整潜在混杂因素后,组间差异仍然显著。
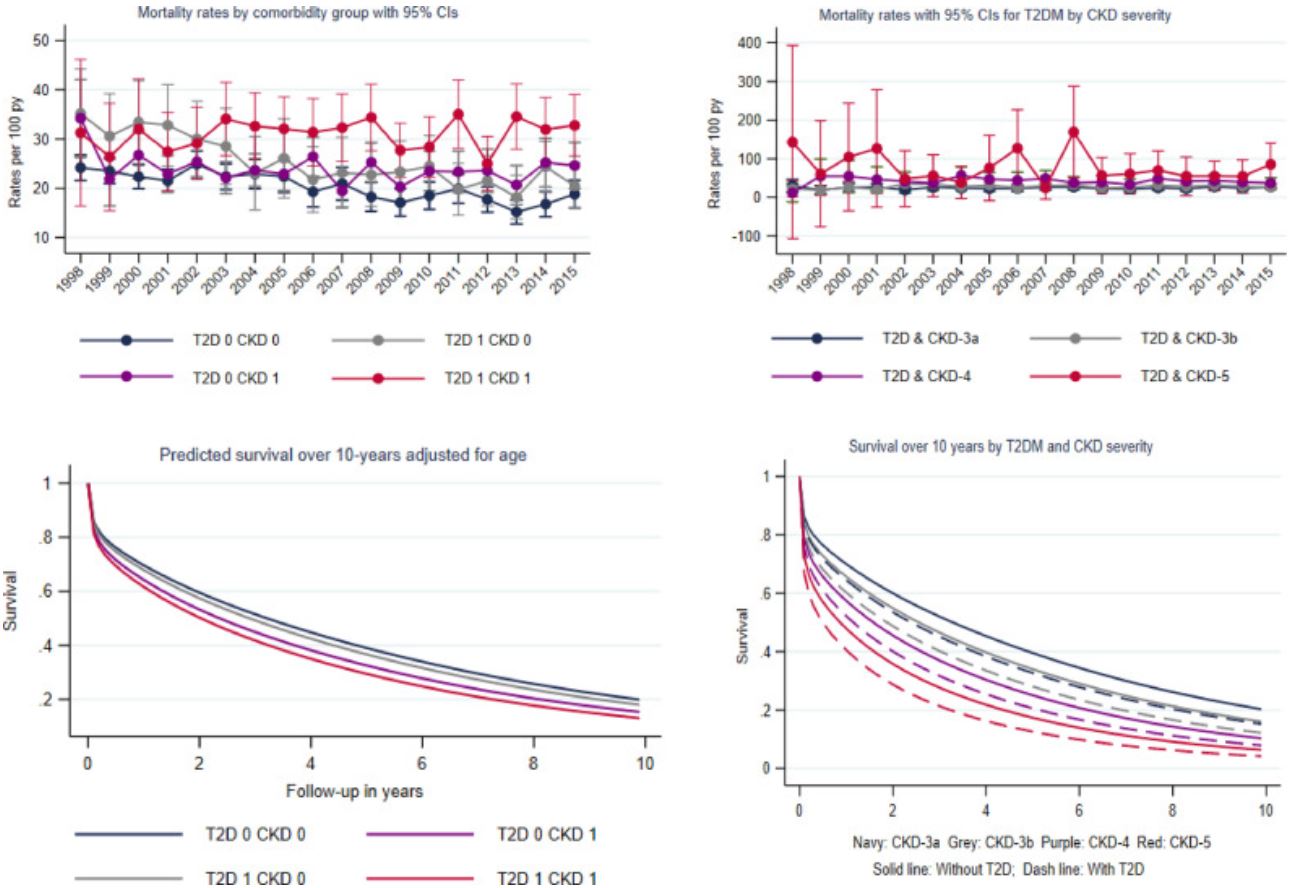
有无糖尿病的患者的死亡率和存活预后趋势变化
对照组和HF-T2D组的患者的中位存活期最长(4.4年和4.1年),而HF-CKD组的只有2.2年。HF-T2D-CKD组的患者的存活期波动在2.8年(CKD-2a)到0.7年(CKD-5)。随着时间的推移,HF-CKD组的CVD住院率显著增加(+26%),HF-T2D组的CVD住院率显著降低(-24%);HF-T2D-CKD任何亚组的CVD住院率均无明显降低。非CVD住院率和死亡率也有相似的趋势:HF-T2D组患者的死亡率显著降低(-37%),HF-T2D-CKD组任何亚组也都无增加。
在新发HF的患者队列中,合并T2D或CKD的HF患者的住院率和死亡率均较高,同时合并T2D和CKD的患者的预后最差。虽然随着时间的推移,HF患者和合并T2D的HF患者预后结果有所改善,但在合并CKD的HF患者中未观察到类似的趋势。
原始出处:
Claire A Lawson, et al. Outcome trends in people with heart failure, type 2 diabetes mellitus and chronic kidney disease in the UK over twenty years. EClinicalMedicine. February 03, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CIN#
61
#DIC#
41
很实用
97
#心衰患者#
43
#clinical#
44
#Medicine#
38
#Med#
44
谢谢MedSci提供最新的资讯
55