Movement disorder:-帕金森患者,大脑代谢和步态有何关系?
2022-06-21 Freeman MedSci原创
两个新的与步态有关的大脑网络,在静止状态下葡萄糖代谢发生了改变
步态困难在帕金森病(PD)中很常见,并导致严重的残疾。它们与跌倒风险的增加和生活质量的降低有关。尽管有最佳的药物治疗,但这些症状会随着疾病的严重程度而逐渐恶化,目前没有具体的治疗方法。
图1: 论文封面图
多巴胺替代疗法(DART)构成了治疗的主流,为选定的步态特征提供了短暂的改善,如步态速度,但会使其他特征恶化,如步态变异性。由于对多巴胺能药物的反应有限,人们提出了影响PD行走神经控制的其他系统。此外,认知障碍已被证明与患者的早期步态障碍有关。
最近的研究表明,步态障碍在PD的前驱阶段也很明显,导致人们对步态特征作为早期疾病识别和监测的生物标志物的潜力产生兴趣。尽管如此,不同步态参数的神经机制仍然难以捉摸,需要为这种疾病的离散步态问题提供可靠的神经影像生物标志物。
尽管步态速度可作为步态完整性的整体测量,但概念性的步态模型已被精心设计,最近的工作表明,在不同的步态领域(如步伐和变异性)所包含的离散步态特征与健康老年人的选择性脑区和网络有关。然而,在PD中,尚不清楚是否存在与特定步态特征(如步态变异性、不对称性或与姿势控制有关的特征)相映射的离散神经网络,以及这些特征在PD患者中如何受到影响。
[18F]-2-氟-2-脱氧葡萄糖-正电子发射断层扫描(FDG-PET)和缩放子轮廓模型/主成分分析(SSM/PCA),一种多变量空间协方差模式分析,已被用于成功地得出与运动障碍、震颤和认知有关的PD代谢轮廓,这些轮廓似乎被治疗干预所调控。 因此,有人认为,在测试新型抗帕金森病疗法的效果时,对这些代谢图谱中由治疗介导的变化进行量化,有可能提供一个客观的结果测量。
藉此,英国Newcastle大学的Hilmar P. Sigurdsson等人,使用FDG-PET和SSM/PCA方法,通过定位与步态特定参数相关的脑区代谢变化,确定PD患者的独立步态相关脑网络。
核心假设:(1) 步态控制由独立的代谢性步态网络提供服务,这些网络与不同的步态结果独立相关;(2) 这些代谢性步态网络的表达在有步态问题的PD患者中是不同的。
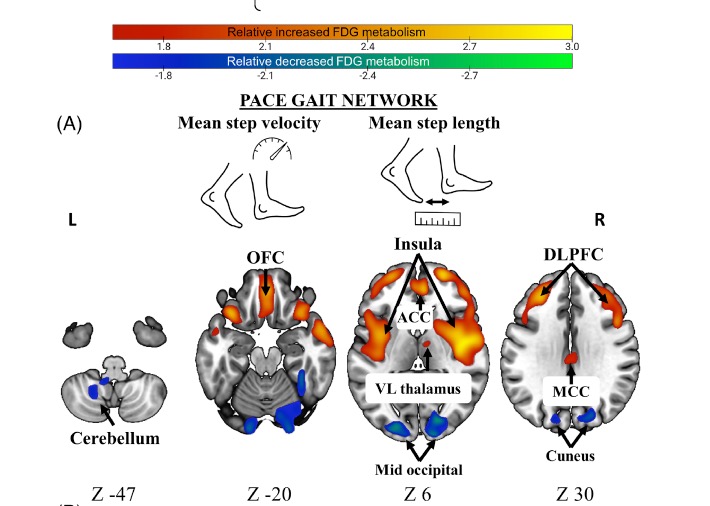
图2:论文结果图
55名早期帕金森病患者和20名年龄匹配的健康志愿者接受了定量步态评估,得出了12个离散的时空步态特征和[18F]-2-氟-2-脱氧葡萄糖-正电子发射断层扫描测量静止的大脑葡萄糖代谢情况。采用多变量空间协方差方法确定与PD离散步态特征有关的脑代谢网络。
在PD中,他们确定了两个与代谢性步态相关的协方差网络。第一个与平均步速和平均步长相关(步伐步态网络),它涉及额叶皮质的相对增加和减少的代谢,包括背外侧前额和眶额、岛叶、辅助运动区、丘脑外侧、小脑和楔叶。
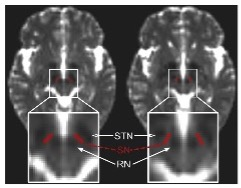
第二个与摆动时间变异性和步态时间变异性相关(时间变异性步态网络),包括感觉运动、顶上皮层、基底节、脑岛、海马、红核和丘脑内侧的代谢相对增加和减少。
相对于健康志愿者,这两个网络的表达在PD患者中明显升高,并且与左旋多巴的剂量或运动严重程度无关。
该研究的重要意义在于发现了两个新的与步态有关的大脑网络,在静止状态下葡萄糖代谢发生了改变。这些步态网络可以作为PD步态障碍的潜在神经影像学生物标志物,并促进这些致残症状的治疗策略的发展。
原文出处:
Sigurdsson HP, Yarnall AJ, Galna B, et al. Gait‐Related Metabolic Covariance Networks at Rest in Parkinson’s Disease. _Movement Disorders_. Published online March 14, 2022:mds.28977. doi:[10.1002/mds.28977](https://doi.org/10.1002/mds.28977)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#脑代谢#
44
#Disord#
56
#Dis#
37
#disorder#
45
#步态#
47
时刻学习
44