IBD: 维多珠单抗的组织浓度与炎症性肠病的粘膜炎症呈相关关系
2021-10-23 MedSci原创 MedSci原创
维多珠单抗 (VDZ) 是一种人源化单克隆抗α4β7 整合素,已被证明是溃疡性结肠炎 (UC) 和克罗恩病 (CD) 的有效治疗药物。
维多珠单抗 (VDZ) 是一种人源化单克隆抗α4β7 整合素,已被证明是溃疡性结肠炎 (UC) 和克罗恩病 (CD) 的有效治疗药物。对药物血清水平较低的患者出现的反应丧失进行剂量优化已被证明是一种有效的策略,可以使接受抗肿瘤坏死因子 (TNF)α 治疗的患者重新获得治疗反应。但是维多珠单抗(VDZ)暴露与治疗反应之间的关联尚不清楚,似乎无法通过血清水平来充分解释。本研究的目的是评估血清和肠道组织中VDZ浓度与粘膜炎症和患者对VDZ反应的关联。
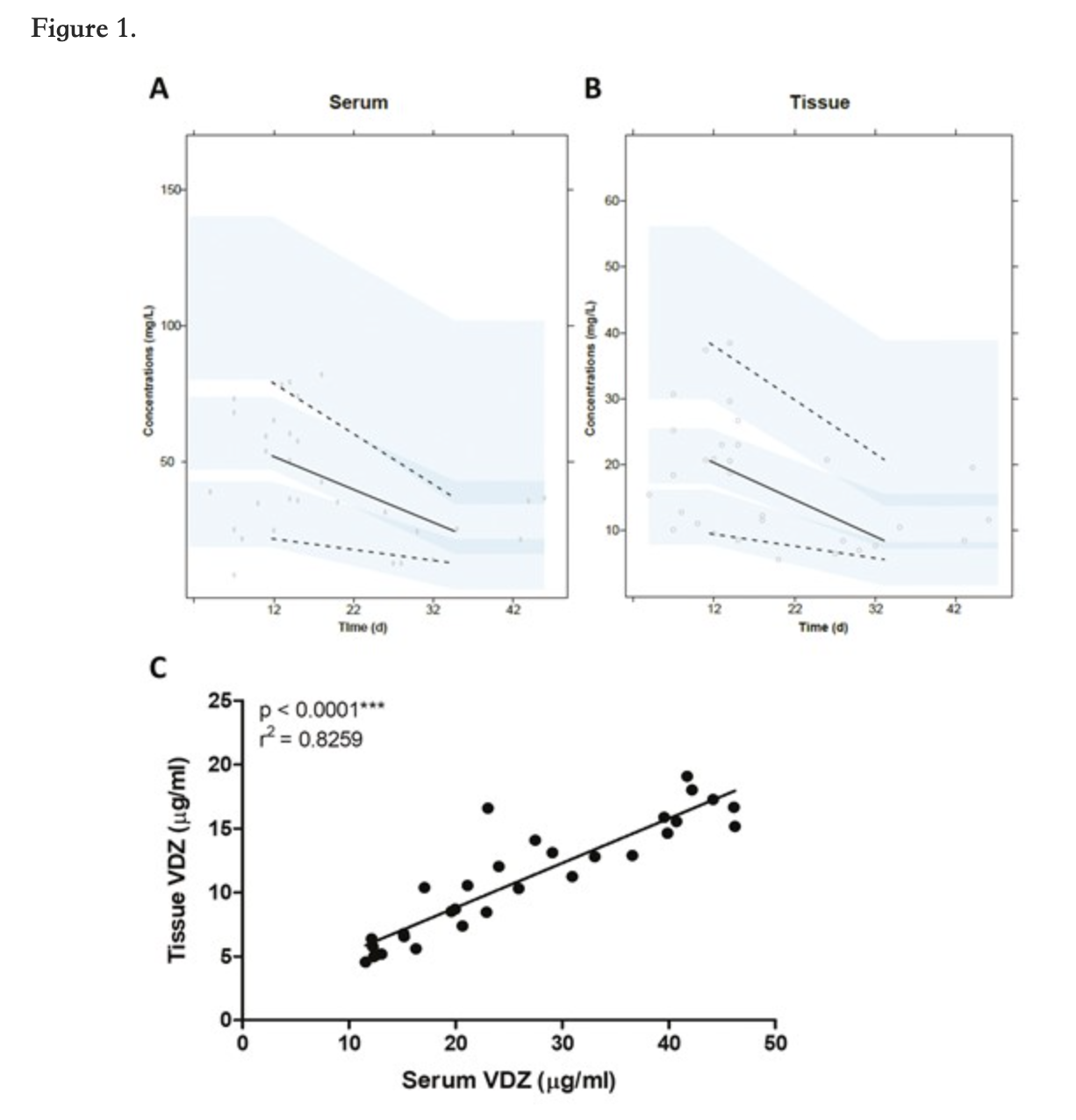
这项前瞻性研究包括37名患有炎症性肠病且基线时有粘膜炎症的成年IBD患者,他们开始使用 VDZ的第16周,通过酶联免疫吸附测定收集血清和活检组织中的VDZ含量。非线性混合效应模型用于计算血清谷浓度和评估肠组织浓度相关性。经验证的临床和内窥镜评分用于定义临床和内窥镜反应和缓解,粪便钙卫蛋白水平用于评估生化反应程度。组织学缓解由 Nancy评分确定。
研究结果显示在血清和组织中观察到 VDZ 浓度与其他部位之间的药物浓度呈正相关(r2=0.83;P<0.0001)。高黏膜VDZ水平而非血清VDZ 水平与黏膜炎症的降低 ( P=0.06) 相关。此外,生化和内镜检查结果显示处于疾病活动期的阳性的患者组织中 VDZ 水平高于静止期的患者(P<0.01)。
本项研究证实VDZ的组织中的浓度水平可能是反IBD患者第16周粘膜炎症和客观治疗结果的标志物。
原始出处:
Renske W M Pauwels. Et al. Vedolizumab Tissue Concentration Correlates to Mucosal Inflammation and Objective Treatment Response in Inflammatory Bowel Disease. Inflammatory Bowel Diseases.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粘膜#
39
#相关关系#
48
#IBD#
38
#浓度#
59
#炎症性#
55
对药物血清水平较低的患者出现的反应丧失进行剂量优化已被证明是一种有效的策略,可以使接受抗肿瘤坏死因子 (TNF)α 治疗的患者重新获得治疗反应
52