李建军:药物机制是PCSK9抑制剂临床获益的有力保证
2018-09-04 MedSci MedSci原创
追本溯源:动脉粥样硬化本质是脂质参与的炎症反应 ESC 2018上,动脉粥样硬化(AS)的发病机制和干预策略再次成为学者们关注的焦点。一方面,LDL-C在AS进程中的核心作用得到了不断积累的证据支持。机制研究显示,LDL-C对AS的作用贯穿AS斑块形成、进展和结局的始终,主要表现为增加斑块的不稳定性,最终导致斑块破裂和血栓形成。ESC 2018上报告的一项纳入超过200万受试者、2000

追本溯源:动脉粥样硬化本质是脂质参与的炎症反应
ESC 2018上,动脉粥样硬化(AS)的发病机制和干预策略再次成为学者们关注的焦点。一方面,LDL-C在AS进程中的核心作用得到了不断积累的证据支持。机制研究显示,LDL-C对AS的作用贯穿AS斑块形成、进展和结局的始终,主要表现为增加斑块的不稳定性,最终导致斑块破裂和血栓形成。ESC 2018上报告的一项纳入超过200万受试者、2000万患者-年随访和15万例心血管事件的荟萃分析显示,无论对于随机对照研究、孟德尔随机化研究还是前瞻性观察性研究,LDL-C水平和心血管事件风险均呈显著的线性关系。 另一方面,AS炎症学说拓展了我们对缺血性心脏病系统性管理的视角。AS是具有慢性炎症反应特征的病理过程,AS的发生和发展始终伴随炎症反应,C反应蛋白(CRP)、白细胞介素-1β(IL-1β)、白细胞介素-6(IL-6)等炎症介质及相关信号通路被证实在AS进程的上游发挥作用,显著增加斑块进展、不稳定性和心血管事件的风险。 由此可见,我们需要从LDL-C的核心作用和炎症反应的基础环境出发,针对关键靶点选择干预策略,有效降低LDL-C水平并抑制炎症反应相关环境,才能真正达到防治AS的目的。
PCSK9是近10余年来发现的AS最新干预靶点之一。PCSK9是一种由肝脏合成的分泌型丝氨酸蛋白酶,能够与LDLR结合,介导后者进入肝细胞后至溶酶体降解,导致肝细胞表面的LDLR数量减少,从而使其对LDL-C分子的摄取和清除能力下降,最终表现为血浆LDL-C水平升高(Figure1)。因此,下调PCSK9的表达、抑制PCSK9的功能是降低LDL-C的有效途径(Figure2)。
Figure 1 PCSK9的作用机制
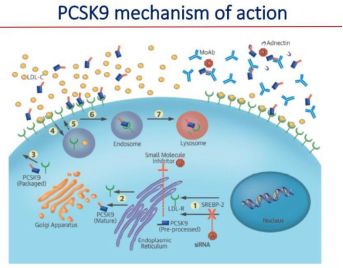
Figure 2 PCSK9的多重抑制途径
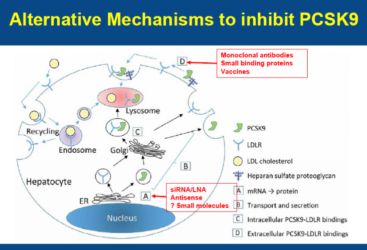
PCSK9单克隆抗体(mAb)抑制剂可以和PCSK9中与 LDLR相互作用部位的临近区域结合,从而阻止 PCSK9 与LDLR的相互作用,使LDL-C更多地被LDLR清除,主要包括依洛尤单抗等。既往研究从分子水平证实,抑制PCSK9表达能够有效降低 LDL-C,并且这种作用是强效且深远的。
首先,PCSK9抑制剂强效降脂,有效干预了AS核心机制。以依洛尤单抗为例,从早期临床试验到近期发表的FOURIER研究等均证实,依洛尤单抗能够在他汀强化调脂治疗基础上进一步显著降低LDL-C水平,显示出PCSK9抑制剂的机制优势。ESC 2018上有学者指出,降LDL-C治疗需“量体裁衣”,在制定LDL-C目标值的基础上,个体化评估患者的危险分层和心血管剩余风险,并通过药物联合、剂量滴定等方式实现LDL-C达标,以实现更多心血管获益。
其次,PCSK9抑制剂可能一定程度上干预了AS炎症反应,进一步实现血管获益。2018年发表的FOURIER最新研究结果显示,LDL-C和hsCRP均与主要终点独立相关,无论基线hsCRP水平如何,依洛尤单抗均有显著的心血管获益,其中基线hsCRP水平较高的患者绝对风险降低幅度更大。
最后,PCSK9抑制剂的靶向干预也是安全性的保证。目前临床应用的PCSK9抑制剂为mAb、注射剂型,用药方案简便。ESC 2018上报告的一项真实世界研究显示,PCSK9抑制剂应用1年的不良事件率低,患者的依从性良好。
另辟蹊径:PCSK9抑制剂通过多重机制改善心血管预后
首先,PCSK9抑制剂针对多重血脂指标,可能实现更多获益。ESC 2018上学者提出,除LDL-C外,脂蛋白a[Lp(a)]、甘油三酯(TG)、HDL-C等指标均与心血管事件相关,也可能作为AS风险评估和疗效评价的替代指标。ESC 2018上报告的研究提示,PCSK9抑制剂能够显著降低Lp(a)水平,高TG血症患者接受PCSK9抑制剂治疗后也可获得更大的TG降幅。可见,抑制PCSK9是血脂谱长期管理的重要策略。
其次,PCSK9抑制剂可能通过减轻缺血/再灌注(I/R)损伤实现心肌保护。在心脏I/R期间,血浆PCSK9水平的升高可能促进炎症和氧化等病理过程,进一步导致心功能障碍。ESC 2018上报告的一项研究通过构建I/R动物模型显示,在缺血损伤前即刻给予PCSK9抑制剂可减少心肌梗死面积、提高左室射血分数,从而发挥心脏保护作用(Figure3)。
Figure 3 PCSK9抑制剂减少心肌梗死面积
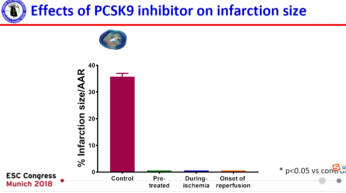
同时,PCSK9抑制剂还能进一步延迟首次心室颤动的发作时间,减轻心律失常易感性。如果仅于再灌注前给予PCSK9抑制剂,则无法实现上述获益。机制研究进一步发现,PCSK9抑制剂能够促进连接蛋白43的磷酸化水平,同时能够降低线粒体活性氧水平、抑制线粒体去极化并减轻线粒体肿胀。PCSK9抑制剂可能通过上述机制,改善I/R导致的心肌损伤和减少心律失常风险,进一步改善左室功能,可见缺血损伤前抑制PCSK9水平即可产生显著获益。
总 结
最后,PCSK9抑制剂未来的发展前景广阔。一方面,随着对PCSK9降解LDLR作用机制的深入理解,调节PCSK9与LDLR结合新的分子途径包括PCSK9小分子干拢RNA(Inclisiran)和PCSK9疫苗(AT04A)等仍在不断探索中,为有效抑制PCSK9提供更多策略。另一方面,抗炎策略的心血管获益也初见端倪,2017年发表的CANTOS研究显示,应用IL-1β的mAb可降低既往心肌梗死患者的炎症标志物水平,进而实现心血管获益。因此,降LDL和抗炎治疗可能通过PCSK9抑制剂为基础的治疗策略实现,成为AS防治未来的方向。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PCSK9抑制#
52
#抑制剂#
54
#PCS#
59
#临床获益#
49
#Csk#
54
嗯嗯,学习学习。
80
学习了,谢谢分享
77
又是一个潜在的降脂药物!
92