Circulation:新发现证实心肌水肿影响肺动脉高压与心包积液的联系
2022-03-18 刘少飞 MedSci原创
肺动脉压升高会导致心肌间质水肿形成,从而导致心肌间质液通过心外膜渗出到周围的心包空间中。
心包积液是成人肺动脉高压的常见表现,与较高的平均右心房压和全身静脉压相关,但与肺动脉楔压无关。尽管肺动脉高压中的大多数心包积液在血流动力学上并不显著着,但积液的存在和程度都是死亡率增加的预测因素。阐明心肌液体平衡机制的实验研究提供了肺动脉高压和心包积液之间令人信服的机制联系。简而言之,肺动脉压升高会导致心肌间质水肿形成,从而导致心肌间质液通过心外膜渗出到周围的心包空间中。
心肌间质液流动
临床上难以记录心肌间质液量的变化。因此,心肌间质性水肿并不是一种常见的临床疾病。然而,一些临床相关病症和干预措施会导致心肌水肿形成,包括肺动脉高压、全身性高血压和心脏停搏的体外循环。心肌间质液来自冠状动脉微血管的血浆超滤进入间质空间。然后,这种间质液流入毛细淋巴管并通过淋巴系统返回全身静脉。在像心脏这样位于潜在空间内的器官中,间质液也可以通过浆膜渗出液流出(即心肌间质液可以通过心外膜直接流入周围的心包空间)。心包液随后通过淋巴管排出并返回血液循环。
冠状静脉高压导致心肌水肿
大多数组织中的静脉高压确实会增加微血管压力,从而增加微血管滤过率。在心脏中,大部分冠状静脉血流通过冠状窦流入右心房,一些静脉血也通过底静脉流入右心房和右心室。利用这种现象,研究人员通过改变冠状窦压力成功地控制了心肌微血管滤过率。冠状动脉窦高压通过升高微血管静水压力导致心肌间质水肿形成,从而增加心肌微血管对间质空间的滤过。重要的是,这种水肿形成发生在左心室心肌以及右心室心肌中。心肌水肿形成导致心肌淋巴流量显著着增加。因为淋巴系统流入颈部大静脉,全身静脉压代表淋巴流出压力。
肺动脉高压导致心肌水肿
实验诱导的肺动脉高压导致急性和慢性制剂中的心肌间质水肿形成。请注意,这些实验研究只关注增加肺动脉压力对心肌液体平衡的影响,而不是关注以肺动脉高压为特征的疾病的更广泛发病机制。这些研究表明如下。肺动脉高压会增加右心房和右心室的压力,这反过来又会提高冠状静脉窦和底比斯静脉内的压力。这种静脉高压增加了冠状循环内的微血管压力,从而增加了滤入心肌间质空间的速率,导致水肿形成(示意图)。此外,右心压力升高还会导致上腔静脉压力升高,通过阻碍心肌淋巴液流动进一步加剧心肌水肿形成(示意图)。
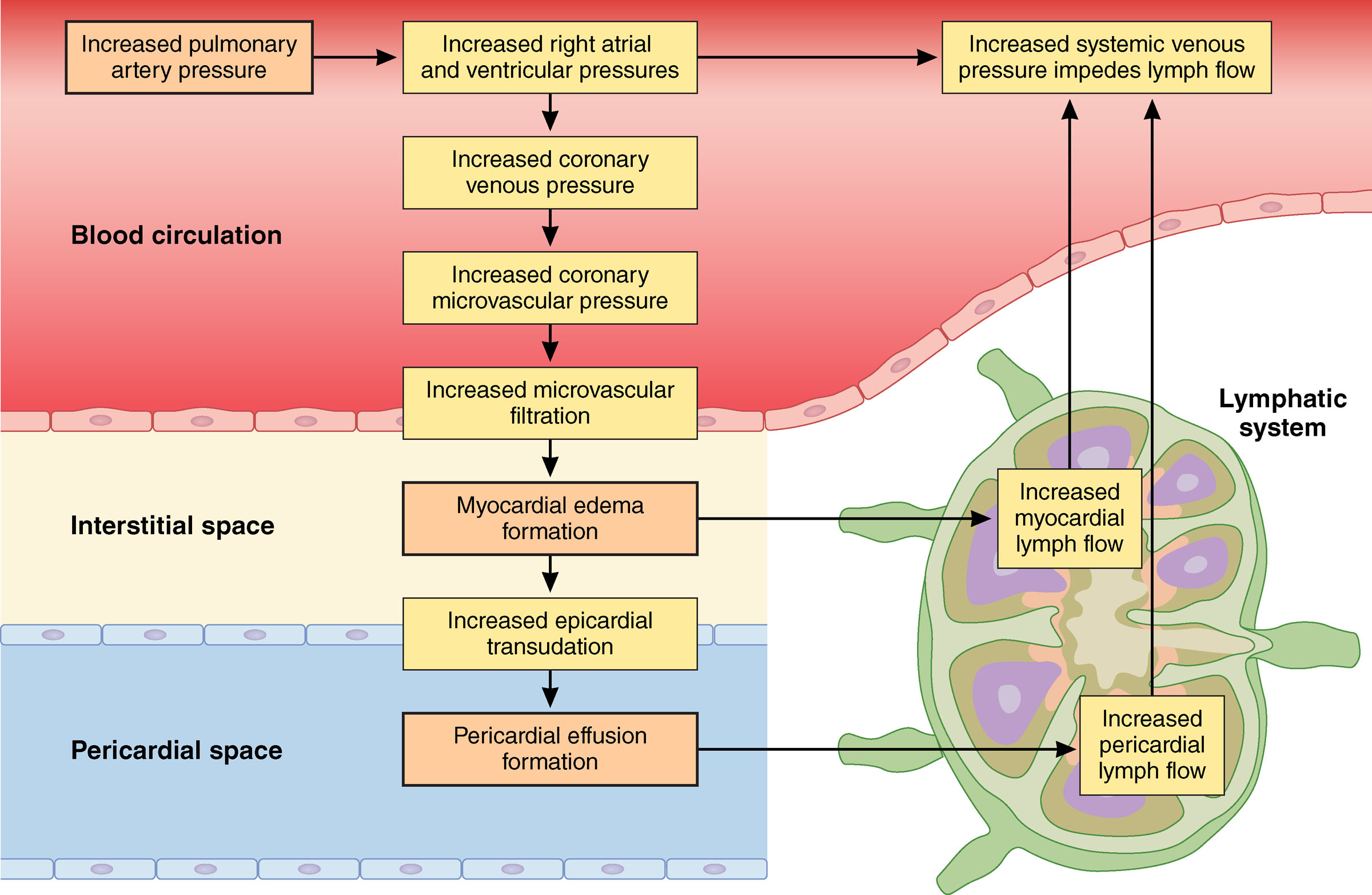
示意图,显著示了肺动脉压力增加后心肌和心包液体平衡的变化。
心肌水肿导致心外膜渗出增加
冠状窦高压的诱发不仅导致心肌水肿的形成,而且还导致更多的心外膜渗出液进入心包腔。这是由于水肿相关的间质压力增加导致间质液通过心外膜进入心包腔。在 Starling-Landis 方程中建模的因素(即间质空间中的静水压力和胶体渗透压)的驱动下,心外膜的流量以可预测的线性方式响应心包液的静水压力和胶体渗透压的变化和心包空间以及心外膜的液体和蛋白质渗透性)。此外,心包液的淋巴引流很可能因全身静脉压升高而减少。
临床意义:
大多数肺动脉高压的心包积液在血流动力学上并不显著着,无需心包穿刺即可治疗,但也可能出现大量积液,偶尔会导致心脏压塞。也可以看到非典型的心包填塞表现,包括孤立的左心房或右心房塌陷和二尖瓣血流的呼吸变化增加。据报道,在这种临床情况下死亡率很高,可能是由潜在疾病和潜在的围手术期并发症引起的。心肌水肿也可能对左心室产生显著着的临床后果,包括心室硬度增加、收缩性降低和长期胶原沉积增加,尽管这些发现的临床意义需要进一步研究。
总之,目前的证据有力地表明,肺血管阻力的增加通过诱导心肌水肿形成而导致心包积液。右心房压力的增加似乎是一个关键的变化,导致冠状静脉和微血管压力增加以及全身静脉压力增加,导致进入心肌间质空间的滤过增加,心外膜渗出增加,以及来自两个血管的淋巴引流受损。心肌间质和心包间隙。
参考文献:
Stewart RH, Cox CS Jr, Allen SJ, Laine GA. Myocardial Edema Provides a Link Between Pulmonary Arterial Hypertension and Pericardial Effusion. Circulation. 2022 Mar 15;145(11):793-795. doi: 10.1161/CIRCULATIONAHA.121.057666. Epub 2022 Mar 14. PMID: 35286166.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#动脉高压#
45
耳目一新
0
#心包积液#
52
#新发现#
50
#学习#学习
101
#心血管#真的很棒
209
#肺动脉高压#
162
#心血管#学习了
202
#水肿#
67