肺动脉高压中扩张的肺动脉压迫左主干冠状动脉的综合分析
2022-03-17 刘少飞 MedSci原创
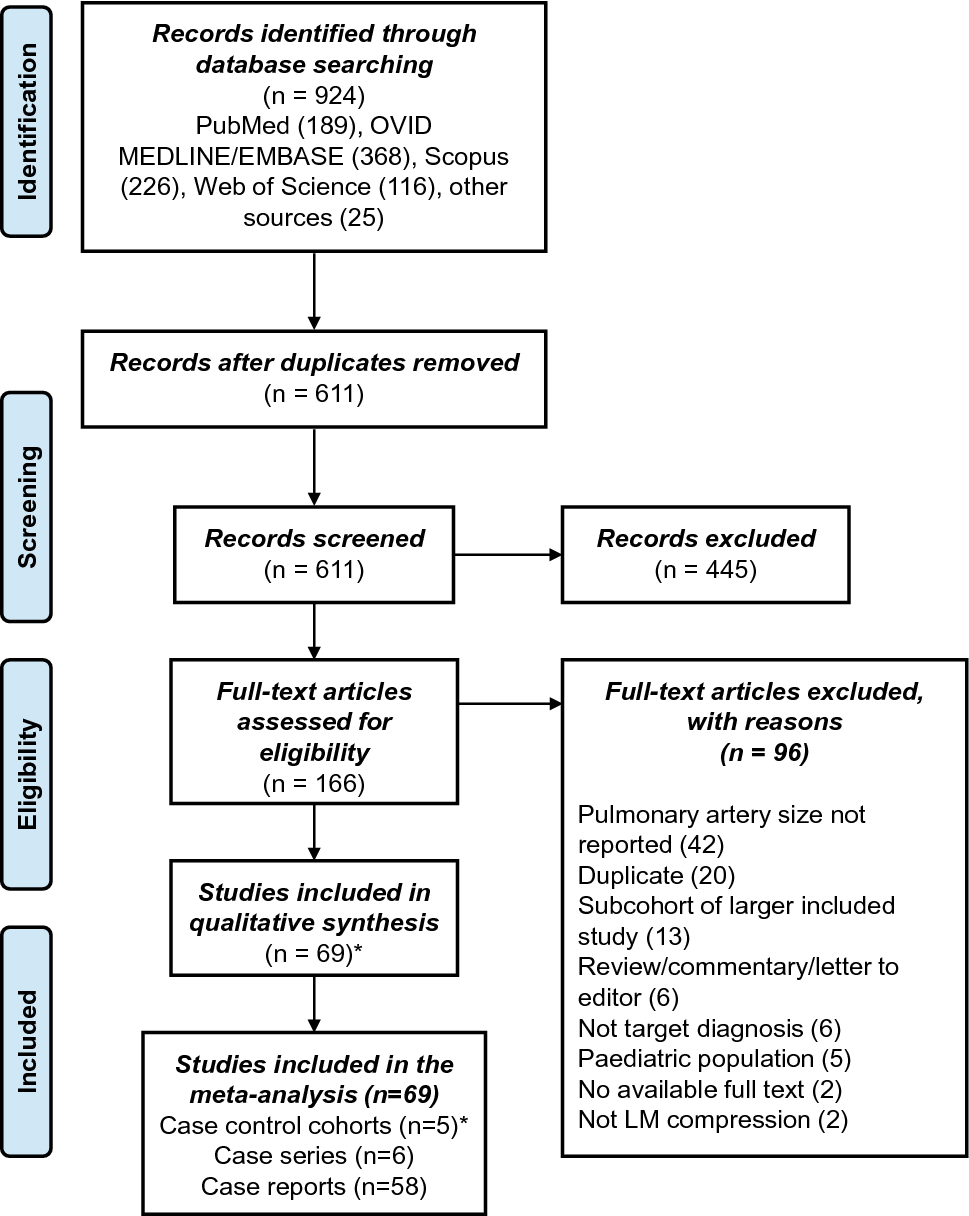
肺动脉高压 (PAH) 可导致左主干冠状动脉受压 (LMCo),但有关影响、筛查和治疗的数据有限。对 LMCo 案例的荟萃分析可以填补该主题的知识空白。
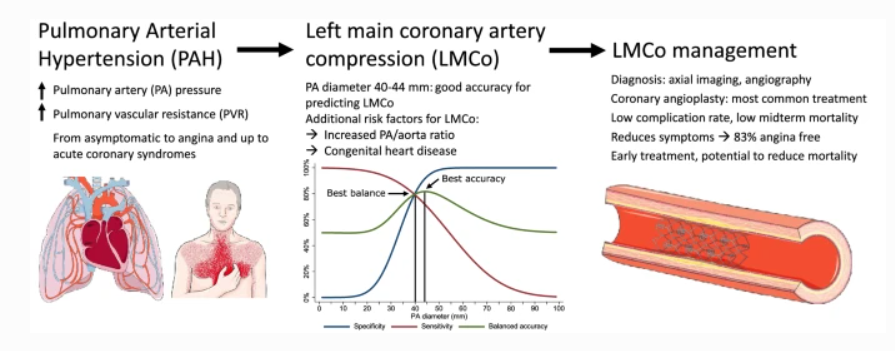
肺动脉高压 (PH) 是一种罕见的综合征,每十万人中的患病率为 1.5-6,其特征是平均肺动脉压 (mPAP) ≥ 25 mmHg。毛细血管前病变或肺动脉高压 (PAH) 的进一步特征是肺血管阻力 (PVR) 和肺楔压正常 增加。尽管最近在管理方面取得了进展,但由于右心衰竭、心源性猝死 (SCD) 或机械并发症, PAH 的预后仍然很差。它是肺动脉 (PA) 扩张的主要原因,进而导致邻近结构的外部压缩,最重要的是左冠状动脉主干 (LMCA)。
LMCA 压迫 (LMCo) 是一种罕见的并发症,估计影响所有 PAH 患者的 6%,以及高达 40% 的有症状患者。关于其临床表现、预测因素和治疗的数据有限,与不良结果相关。PA 直径 > 40 mm 已被提议作为对有症状患者进行 LMCo 筛查的截止值,但这尚未在初始研究之外得到验证 。LMCo 管理的报告仍然很少,并且仅限于小型队列 或单个病例报告。关于 LMCo 筛查和治疗的高质量证据有限,这意味着关于这些主题的建议很少。
为了解决这些知识空白,我们对文献进行了系统回顾和荟萃分析,目的如下: 1. 描述 PAH 中与 LMCo 相关的临床、血流动力学和影像学参数;2. 确定影像学和/或血流动力学参数在 LMCo 筛查中的作用,并确定其最佳临界值;3. 评估 LMCo 在 PAH 中的治疗方案及其结果。
干预和结果:
共有 150 例 LMCo 病例接受了非保守治疗:115 例接受了 PCI,8 例接受了 CABG,10 例接受了 PA 重建/扩张。干预后中期有 4 人死亡,死亡率为 2.7%,平均/中位随访时间为 17 至 22 个月。只有一项研究详细说明了干预后更长的随访时间,报告平均随访 4.5 年时心脏死亡率为 27.5%。具体来说,在接受非保守治疗和可用症状数据的幸存者中(n = 49),41 人(83%)报告干预后没有心绞痛,4 人(8%)有复发性心绞痛、持续性 LMCo 或恶化心脏衰竭。
研究启示:
需要将 PAH 患者的标准化 LMCo 筛查方案纳入常规随访建议中。建议的 40-44 毫米的 PA 直径截止值提供了良好的诊断准确性,可用于指导转诊以进行确认成像研究。PAH 的病因、症状和 PA/主动脉比率也应包括在风险评估评估中。金标准诊断仍然是冠状动脉造影,而侵入性较小的 CT 血管造影是一个值得注意的替代方案。非保守治疗,即 PCI,在减轻心绞痛方面是安全有效的,但目前的数据尚不清楚对降低死亡率的真正影响。未来的研究应侧重于评估系统筛查 LMCo 联合常规 PCI 对这些患者的益处。
参考文献:
Badea, R., Dorobantu, D.M., Sharabiani, M.T.A. et al. Left main coronary artery compression by dilated pulmonary artery in pulmonary arterial hypertension: a systematic review and meta-analysis. Clin Res Cardiol (2022). https://doi.org/10.1007/s00392-022-01999-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#扩张#
43
#动脉高压#
44
#左主干#
46
#动脉压#
35
#肺动脉压#
49