Movement disorders:帕金森病的运动和认知代谢网络之间的关系
2022-08-30 Freeman MedSci原创
通过delta量化的PDRP优势,可以检测出PD患者的功能障碍从运动网络向认知网络的扩散
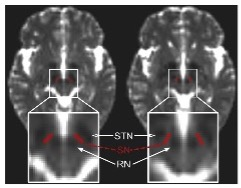
尽管特发性帕金森病(iPD)患者的症状表现和疾病进展各不相同,但基本的组织病理学变化和所涉及区域的时间顺序是相对定型的。iPD与两个不同的代谢网络有关,即PD相关模式(PDRP)和PD相关认知模式(PDCP),它们分别与该疾病的运动和认知表现有关。用[18F]-氟脱氧葡萄糖(FDG)正电子发射断层扫描(PET)进行的纵向成像研究表明,PDCP在运动发病后4至6年开始明显升高。因此,与PDCP相比,在同一病人身上测量PDRP时,预计PDRP会有优势的表达。
 图1: 论文封面图
图1: 论文封面图
在这种情况下,PDRP的优势可以从Braak最初描述的iPD的组织病理学变化的区域顺序来理解。疾病相关网络的异常甚至可能早于运动症状的出现,这一点从特发性快速眼动睡眠行为障碍(iRBD)患者的PDRP升高可以看出,这是一种前驱形式的疾病。相反,在非典型帕金森综合征(APS)中,如多系统萎缩(MSA)和进行性核上性麻痹(PSP),PDRP不可能占优势,Braak的顺序并不适用。
在这项研究中,斯洛文尼亚UMC Ljubljana的Tomaz Rus 等评估了不同病程的iPD患者的多个样本的PDRP优势,这些患者在四个不同的部位进行了FDG-PET扫描。对于每个病人,他们测量了PDRP和PDCP的表达水平,并计算了这些数值的差异,这被称为delta。我们研究了横断面iPD样本中delta与疾病持续时间的关系以及随着时间的推移。
同样,将iPD患者的delta与iRBD19受试者以及与LRRK2-G2019S突变相关的PD基因型和与疾病进展缓慢和更快相关的GBA1变体患者的相应数值进行比较。所得数据与APS患者中获得的相应措施进行了比较。最后,作为原则性证明,使用静止状态fMRI(rs-fMRI)非侵入性地获得类似的结果,证明了delta更广泛的应用潜力。
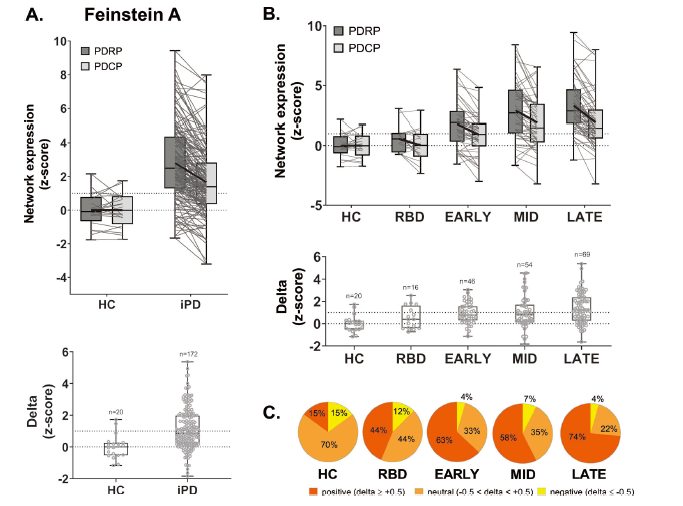
图2:论文结果图
他们使用[18F]-氟脱氧葡萄糖正电子发射断层扫描和静息态fMRI来量化delta,并比较不同样本的测量结果;同样在纵向的病人样本中评估delta随时间的变化。最后,评估了iRBD前驱个体和gPD受试者的delta。
四个iPD样本中的每一个Delta都异常升高(P < 0.05),在有风险的iRBD组中也是如此(P < 0.05),其数值随时间的推移而增加(P < 0.001)。
PDRP的优势也存在于gPD中,与侵略性较弱的LRRK2-G2019S突变相比,GBA1变体患者的数值更高(P = 0.005)。
这一趋势在非典型帕金森综合征患者中没有观察到,根据PDRP的表达和delta(曲线下面积=0.85;P < 0.0001),他们与iPD的区别很准确。
该研究的重要意义在于发现了:通过delta量化的PDRP优势,可以检测出PD患者的功能障碍从运动网络向认知网络的扩散。因此,Delta可能有助于鉴别诊断和跟踪个别患者的疾病进展。
原文出处:
Rus T, Schindlbeck KA, Tang CC, et al. Stereotyped Relationship Between Motor and Cognitive Metabolic Networks in Parkinson’s Disease. _Movement Disorders_. Published online August 23, 2022:mds.29188. doi:[10.1002/mds.29188](https://doi.org/10.1002/mds.29188)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Dis#
62
#disorder#
52
#Disord#
40
#ERS#
37
#disorders#
40