Eur Heart J:残余胆固醇可预测心血管疾病
2021-07-24 MedSci原创 MedSci原创
在无ASCVD的个体中,升高的RC水平与ASCVD相关,且独立于传统的危险因素、LDL-C和apoB水平。
新出现的证据表明,残余胆固醇(RC)会促进动脉粥样硬化性心血管疾病(ASCVD)。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员旨在评估无ASCVD的患者相比于低密度脂蛋白胆固醇(LDL-C)和载脂蛋白B(apoB)之外RC的相关风险。
研究人员汇总了来自社区动脉粥样硬化风险研究(n=9748)、动脉粥样硬化的多种族研究(n=3049)和年轻人冠状动脉风险的发展研究(n=4735)的17532名无ASCVD个体的数据。研究人员通过非高密度脂蛋白胆固醇(非HDL-C)减去LDL-C获得RC,并使用调整后的Cox模型来估计与logRC水平相关的ASCVD事件风险。
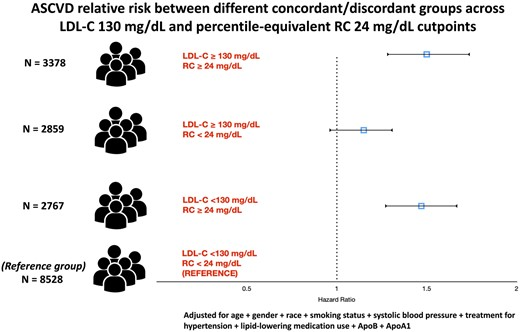
参与者的平均年龄为52.3±17.9岁,56.7%为女性,34%为黑人。在中位随访18.7年期间,共有2143起ASCVD事件。在包括LDL-C和apoB在内的多变量调整后,logRC与较高的ASCVD风险相关[风险比(HR)为1.65,95%置信区间(CI)为1.45–1.89]。此外,与一致组相比,不一致的高RC/低LDL-C组,而不是低RC/高LDL-C组与ASCVD风险增加相关(HR为1.21,95%CI为1.08-1.35)。在评估跨临界点的不一致时也具有类似的结果。
在无ASCVD的个体中,升高的RC水平与ASCVD相关,且独立于传统的危险因素、LDL-C和apoB水平。
原始出处:
Renato Quispe.et al.Remnant cholesterol predicts cardiovascular disease beyond LDL and ApoB: a primary prevention study.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab432
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习了,谢谢!
52
学习了,设计研究模型
57
增长了知识,謝謝!
63
#残余胆固醇#
42
#ART#
38
#血管疾病#
31
#HEART#
33
非常受用
58
非常受用
56
学习啦~谢谢
47