ACR 2021——30年了!ACR血管炎标准终于更新了!
2021-11-17 彼岸边草 MedSci原创
目前临床上采用的血管炎分类标准还是1990年的ACR标准。旧标准已经不能够很好的辅助临床的诊疗,血管炎亟待一个新的标准。于今年刚结束的ACR大会上,发布了最新的2022年的血管炎分类标准。
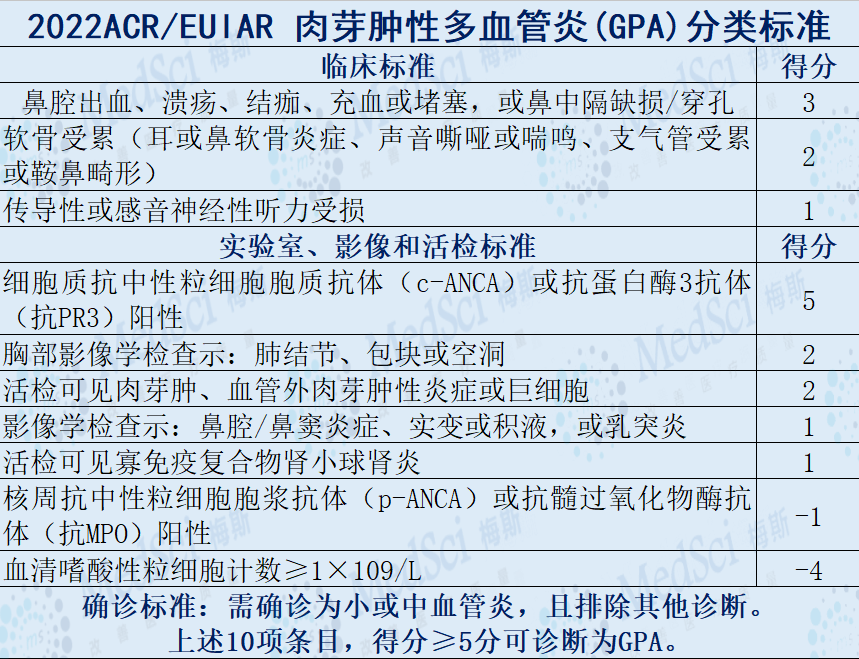
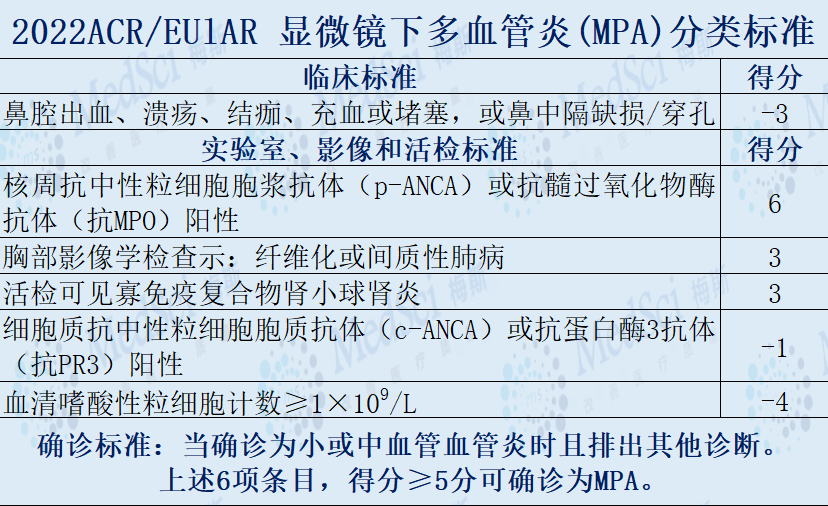
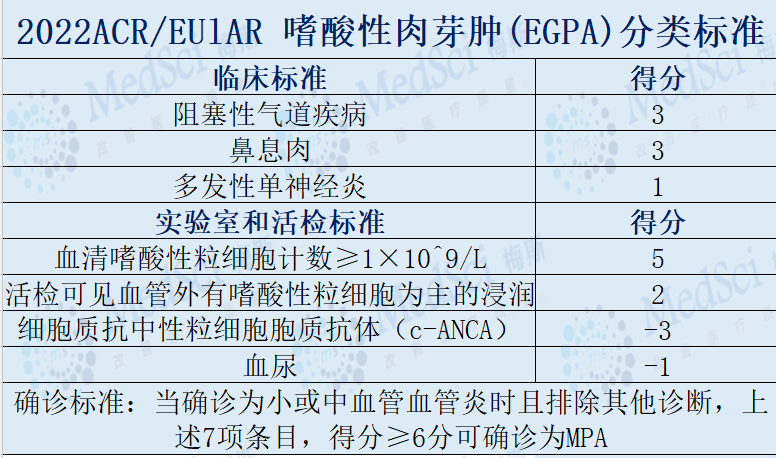
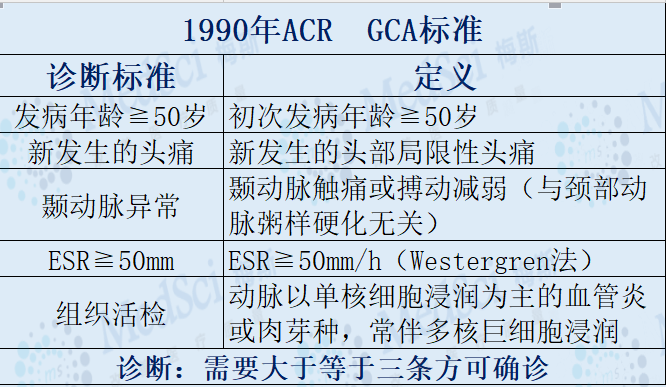
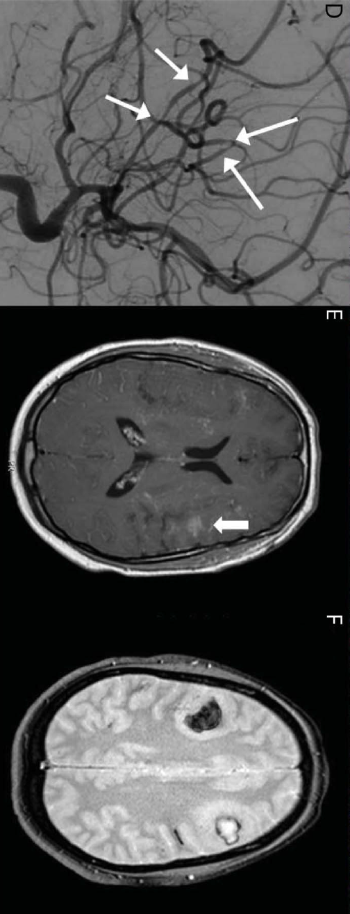
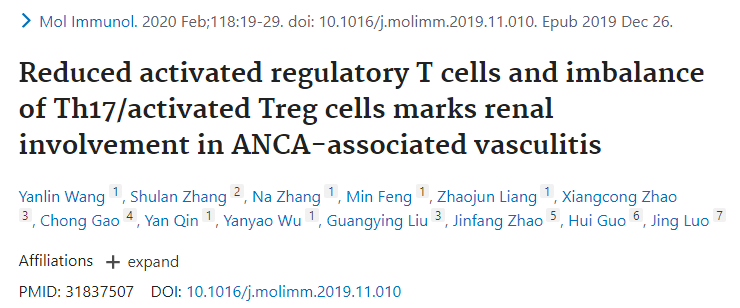
血管炎是指血管壁中存在炎性细胞,对血管壁结构有反应性损伤。血管完整性丧失(导致出血)和管腔受损都可能导致下游组织缺血和坏死。血管炎的确切发病机制尚不清楚。 目前血管炎的分类还依赖于1990年ACR制定的分类标准,一般来说,受累血管的大小、类型和位置与特定类型的血管炎有关。但毕竟标准使用了30多年,已经逐渐不能满足临床需求。 1990年ACR分类标准的局限性 最新的研究队列显示,旧指南的敏感性较低 鉴于此,在美国当地时间11月3日至11月9日召开的美国风湿病学会(ACR)年会上,ACR与欧洲抗风湿病联盟(EULAR)联合发布《2022年版血管炎分类标准》,标准涉及抗中性粒细胞胞质抗体(ANCA)相关性血管炎(AAV)(肉芽肿性多血管炎[GPA]、显微镜下多血管炎[MPA]和嗜酸性肉芽肿性多血管炎[EGPA])和大血管炎(巨细胞动脉炎[GCA]、大动脉炎[TAK])等多个类型的血管炎。 新发布的2022ACR/EULAR分类标准是迄今为止最大规模的血管炎的研究,共纳入了1400多例病例,同时也纳入了除了北美外的数据,覆盖32个国家的136个中心。同时新的影像学检查技术也被纳入到分类标准中来,希望能够满足当代血管炎诊疗的需要。 ANCA相关性血管炎(AAV) AAV是一种坏死性血管炎,无明显免疫复合物沉积,与髓过氧化物酶特异性ANCA(MPO-ANCA)或蛋白酶3特异性ANCA(PR3-ANCA)相关。主要累及小血管(小动 脉、微小动脉、微小静脉和毛细血管),也可有中血管受累。 ANCA阴性AAV类似于血清阴性红斑狼疮或血清阴性类风湿性关节炎,患者满足AAV的诊断,但ANCA血清学检测结果为阴性。AAV患者ANCA阴性可能因为当前方法尚无法检测到,或可能具有尚未发现的特异性ANCA,或致病因素与ANCA阳性无关。不同于小血管动脉炎特征性的中度至大量血管壁免疫沉积物,血管壁少或无免疫沉积物是AAV的主要特征。 肉芽肿性多血管炎(GPA) 肉芽肿性多血管炎(GPA)是一种主要累及中小血管(例如毛细血管、小静脉、小动脉、动脉和静脉)的坏死性血管炎。它通常会导致上呼吸道和下呼吸道的肉芽肿性血管炎,以及坏死性寡免疫复合物肾小球肾炎。80% 以上的 GPA 患者存在 ANCA。 新标准的的敏感性92%、特异性94%。 显微镜下多血管炎(MPA) MPA是一种坏死性血管炎,主要累及毛细血管、微静脉或微动脉,最常见表现为坏死性肾小球肾炎和肺毛细血管炎,中小动脉也可受累。通常无肉芽肿性炎症,可与肉芽肿 性多血管炎相鉴别。90% 以上的 MPA 患者存在 ANCA。 该标准敏感性91%、特异性94%。 嗜酸性肉芽肿性多血管炎(EGPA) 嗜酸性肉芽肿性多血管炎(EGPA) EGPA 是一种组织中嗜酸性粒细胞浸润的肉芽肿性坏死性血管炎,主要累及中小血管,也称为变应性肉芽肿性血管炎、Churg-Strauss 综合征。患者常有过敏性哮喘、慢性鼻-鼻窦炎,外周血嗜酸性粒细胞明显 增多。 大血管炎(LVV) 大血管炎(LVV)中Takayasu动脉炎(TAK)和巨细胞动脉炎(GCA)的组织病理学特征难以区分。两个都主要发生于女性。尽管LVV对大动脉影响很大,特定患者的大动脉可能不是受影响的主要血管类型,因为可能有许多更小分支受影响(尤其是中动脉)。 例如,成像和荧光素血管造影研究表明,巨细胞动脉炎的眼部受累可能影响不仅是眼动脉,还有视网膜动脉和多个睫状动脉(中动脉),甚至睫状动脉和视网膜动脉的较小分支(小动脉)。 大动脉炎(TAK) TAK以女性多见,主要影响主动脉和/或其主要分支血管。发病年龄通常在50岁,这有别于巨细胞动脉炎(通常发生在50岁之后)。 VS 新标准的敏感性为94%,特异性99%。新标准较1990年标准不仅改变了诊断方法:由确诊条目改为积分制。而且放宽了年龄的限制,由40岁改为60岁。 巨细胞动脉炎(GCA) 又称为颞动脉炎,常为肉芽肿性动脉炎。主要累及主动脉及其主要分支,包括颈动脉分支,尤其是颞动脉。通常在50岁之后发病,其中70~90岁个体的发病率显著增加,常伴发风湿性多肌痛。 VS 新标准的颁布,仍然需要更多的数据来验证它的适用性。 参考文献: [1]. Jennette JC, Falk RJ, Bacon PA, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013 Jan;65(1):1-11. doi: 10.1002/art.37715. PMID: 23045170. [2]. Peter Grayson,Raashid Luqmani. New ACR/EULAR Classification Criteria for Vasculitis”ACR convergence 2021,oral presentation.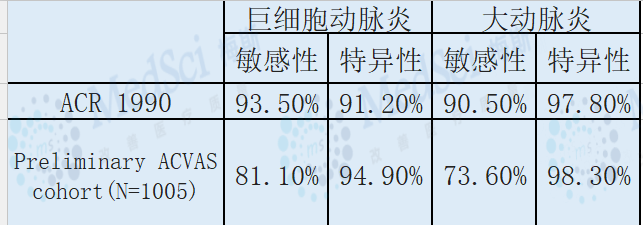




本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习到了
43
学习了
62
#血管炎#
41
#ACR#
0
怎样下载
82
能下载吗
61
棒棒哒
68