AP&T:埃洛比昔巴特在慢性便秘中的作用与粪便脱氧胆酸有关
2020-08-19 MedSci原创 MedSci原创
胆汁酸来源于胆固醇,主要负责脂肪乳化促进小肠中脂质的消化吸收。此外,它们能调节结肠的分泌和运动,从而导致结肠转运改变。
胆汁酸来源于胆固醇,主要负责脂肪乳化促进小肠中脂质的消化吸收。此外,它们能调节结肠的分泌和运动,从而导致结肠转运改变。这些胆汁酸中约有95%通过末端回肠中的根尖钠依赖性胆汁酸转运蛋白(ASBT)重新吸收,而约5%的胆汁到达结肠并受到胆汁盐水解酶(BSH)的解偶联,BSHs的活性会影响宿主和微生物的生理。
埃洛比昔巴特(Elobixibat)是一种新型的ASBT抑制剂,可阻断回肠末端表达的ASBT的作用,并有效治疗慢性便秘。过抑制胆汁酸的重吸收,埃洛比昔巴特增加了到达大肠的胆汁酸的量,随后通过激活Takeda G蛋白偶联受体5(TGR5)增强了结肠的分泌和运动能力。然而,尚不清楚哪种埃洛比昔巴特会增加胆汁酸的浓度,埃洛比昔巴特对胆汁酸的结肠浓度增加如何影响肠道菌群,肠功能的益处是否与胆汁酸改变或胆汁酸改变的功能影响有关?因此,有研究人员对埃洛比昔巴特对粪便中总胆汁酸和个别胆汁酸浓度以及粪便微生物群浓度变化的影响进行了研究。
这是一项前瞻性,单中心研究,该研究于2018年7月至2019年2月从横滨市立大学医院招募了符合标准的便秘患者。患者在2周内每天接受10 mg 埃洛比昔巴特的治疗,试验结束时研究人员评估了依洛昔巴特给药前后对肠道功能,粪便胆汁酸浓度变化和肠道细菌组成的影响。

doi.org/10.1111/apt.15950
在纳入分析的30例患者中,治疗前和治疗后每两周排便的频率分别为7和10(P <0.001)。服用依洛昔巴特后,粪便中总胆汁酸的浓度显着增加。每种胆汁酸都有增加的趋势,治疗前粪便中胆汁酸的浓度从10.9 µg /g增加至治疗后的粪便中的15.0 µg/g(P = 0.030),粪便中的脱氧胆酸显着增加(治疗前粪便3.94 µg / g至治疗后5.02 µg/ g,P= 0.036)。
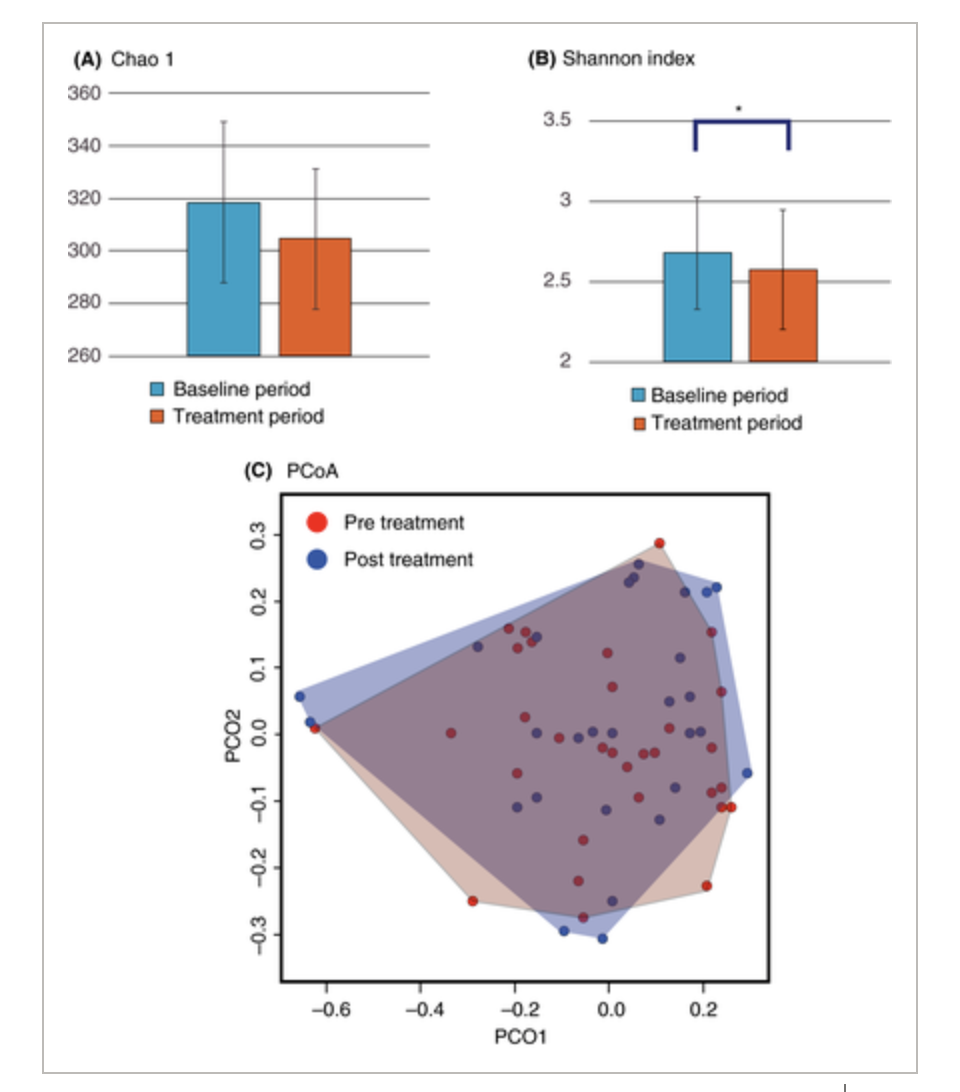
最后研究人员说道在这项研究中,粪便中总胆汁酸和次级胆汁酸的浓度显着增加,并且肠道微生物群的多样性随着依洛昔巴特对慢性便秘患者的治疗而降低。因此依洛昔巴特的生物学作用与其对分泌性胆汁酸的作用有关,而不是与改变的粪便微生物群的结构变化有关。
原始出处:
Noboru Misawa. Et al. The benefit of elobixibat in chronic constipation is associated with faecal deoxycholic acid but not effects of altered microbiota. Alimentary Pharmacology and Therapeutics.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粪便#
44
那多吃点胆固醇类食物,是不是也可以治疗便秘呢?#便秘##胆汁酸#
207
很有用
89
学习了
69
很好
90
!
92
!
43
棒
39
学习一下
23