OCC 2022:值班遇“胸痛”,快速解读D-二聚体
2022-05-30 MedSci原创 MedSci原创
心内科经常要查D-二聚体,那么,D-二聚体在胸痛患者中的临床价值在哪里?
近年来,随着我国人口老龄化加快,急性胸痛患者人数也在逐年增加。据数据显示,急性胸痛约占急诊内科病人5%~20%,三级医院可能会达到20%~30%。
因急性胸痛的临床症状复杂多样,发作急骤,病情迅速恶化,短时间内危及患者的生命。因此,对于急性胸痛患者,快速实验室检查有利于迅速明确诊断、完善评估、指导治疗。
心内科经常要查D-二聚体,那么,D-二聚体在胸痛患者中的临床价值在哪里?上海交通大学医学院附属仁济医院沈节艳教授以“值班遇“胸痛”,快速解读D-二聚体”为题,对相关内容进行了详细的讲解。
胸痛的病因和鉴别
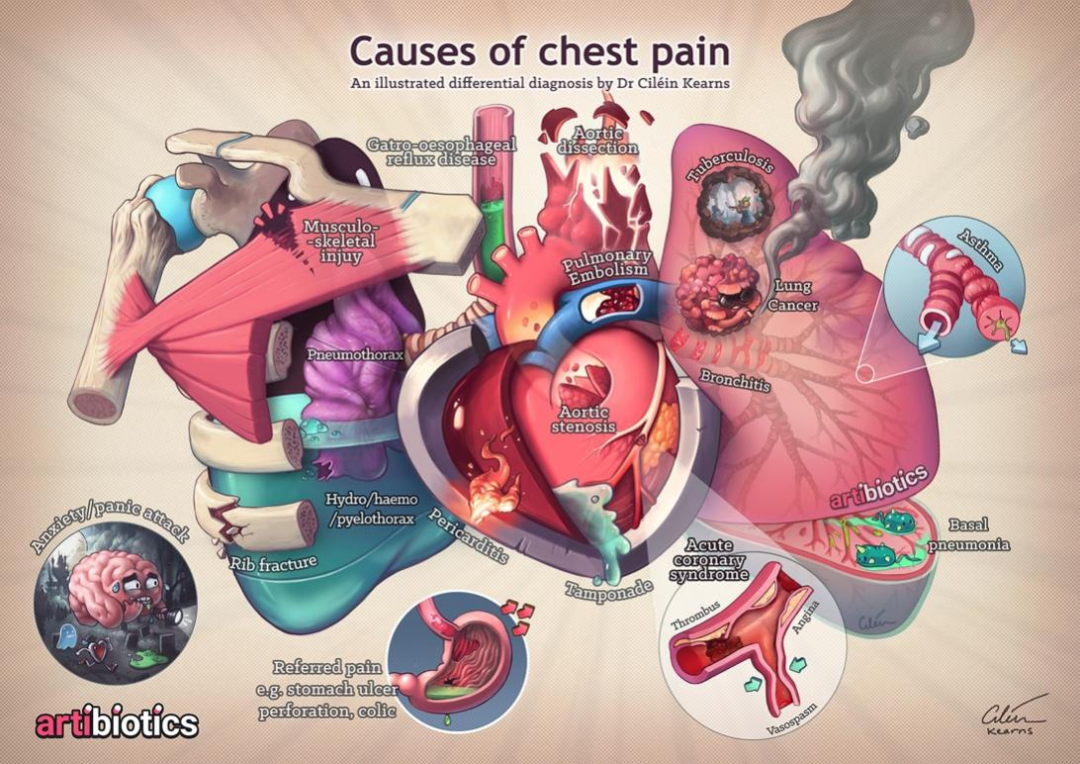
沈节艳教授表示,在我国急诊患者胸痛十大病因中,非心源性胸痛几乎占到50%,排在第二位的心绞痛,第三位是心律失常。

图:常见胸痛部位和病因
在识别心肌缺血性胸痛时,可根据不同的疼痛的性质区分。若疼痛位于中央型,具有压迫感、压榨样、紧绷感或沉闷感等,更加倾向于心肌缺血性胸痛(心绞痛/心梗)。若疼痛具有刀割样、短暂痛、转移痛或胸膜痛等,比较倾向于神经有关。

图:识别心肌缺血性胸痛
致命性胸痛常见的病因包括心源性和非心源性胸痛。心源性胸痛病因包括急性冠脉综合征、主动脉夹层、心脏压塞、心脏挤压伤(冲击伤)、急性肺栓塞等。非心源性胸痛病因有张力性气胸等。
另外,非致命性胸痛常见的病因也分为心源性和非心源性胸痛。心源性胸痛病因包括稳定性心绞痛、急性心包炎、心肌炎、肥厚性梗阻性心肌病等等。非心源性胸痛病因有胸壁疾病、呼吸系统疾病、消化系统疾病和心理精神源性疾病等。
由于基层以老年患者为主,沈节艳教授强调,随着年龄的增加,冠心病是胸痛的重要危险因素,对于大于75岁的胸痛患者来说,出现呼吸困难、晕厥或急性谵妄等伴随症状,或发生不明原因跌倒时,应优先考虑急性冠脉综合征和肺栓塞。
D- 二聚体临床诊断价值
D- 二聚体是急性血栓形成后纤溶系统被即刻激活继而纤维蛋白降解得到的产物。当体内血栓溶解后,D- 二聚体即被释放入血。D- 二聚体反应体内凝血酶/纤维蛋白溶解酶的活性,标志着体内凝血和纤维系统的双重激活。
D- 二聚体在致命性胸痛鉴别诊断中具有很大的价值。由于急性肺栓塞、主动脉夹层和急性冠脉综合征都是血栓性疾病,因此D- 二聚体都可以升高,但是升高比例和幅度却有所不同。
以急性肺栓塞为例,急性肺栓塞临床表现缺乏特异性、临床上容易被漏诊和误诊。在临床上,不明原因的虚脱、面色苍白、出冷汗、呼吸困难者、胸痛、咳嗽等,并有脑缺氧症状如极度焦虑不安、倦怠、恶心、抽搐和昏迷。而急性肺血栓栓塞症是急性肺栓塞最常见的类型。
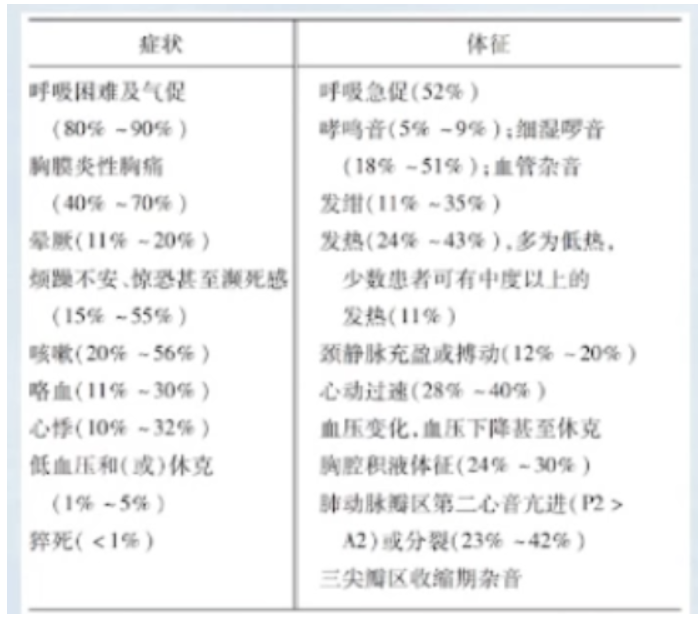
图:急性肺血栓栓塞临床表现
D- 二聚体对急性肺栓塞诊断价值:
1)D- 二聚体约96.4%为阳性,阴性(小于0.5ug/ml)基本可以排除肺栓塞(阴性预测值为99.6%)
2)正常值随着年龄而变化,50岁以上,正常值:年龄*10ug/L
3)D- 二聚体升高范围从0.5ug/ml到40ug/ml以上都有
4)D- 二聚体检测对于中低危肺栓塞患者价值不大。对于高危患者,不建议立即进行D- 二聚体检测,而是要立刻进行床旁超声或CT检查
D- 二聚体可指导溶栓治疗:
1)在溶栓治疗后,D- 二聚体短期内明显上升,而后逐渐下降,提示治疗有效
2)D- 二聚体持续上升或下降缓慢,提示存在新发血栓,溶栓药物剂量不足
3)D- 二聚体变化不大,则可能为陈旧的机化的血栓
D- 二聚体与主动脉夹层:
1)典型的主动脉夹层:即内膜有裂口的主动脉夹层,D- 二聚体几乎100%阳性,因此,D- 二聚体小于0.5ug/ml时几乎可以排除主动脉夹层(阴性预测值约100%)
2)主动脉壁间血肿和溃疡:对于主动脉壁间血肿和溃疡的患者,D- 二聚体有1/3左右正常,因此不能根据D- 二聚体正常而排除主动脉壁间血肿和溃疡
D- 二聚体与急性冠脉综合征:
1)不稳定性心绞痛和急性非ST段抬高型心肌梗死,此类患者D- 二聚体一般不升高
2)急性ST段抬高型心肌梗死,此类患者中D- 二聚体约5%出现阳性(大于0.5ug/ml)一般为轻度升高,很少超过3ug/ml,极少超过5ug/ml(除非血栓自溶或溶栓治疗后)
3)D- 二聚体水平可以预测急性心肌梗死患者的远期预后,D- 二聚体水平升高提示合并其他严重合并症,因此预后更差。
此外,除了急性肺栓塞、主动脉夹层和急性冠脉综合征,D- 二聚体升高常常还见于深静脉血栓、弥漫性血管内凝血、肝病和妊娠。
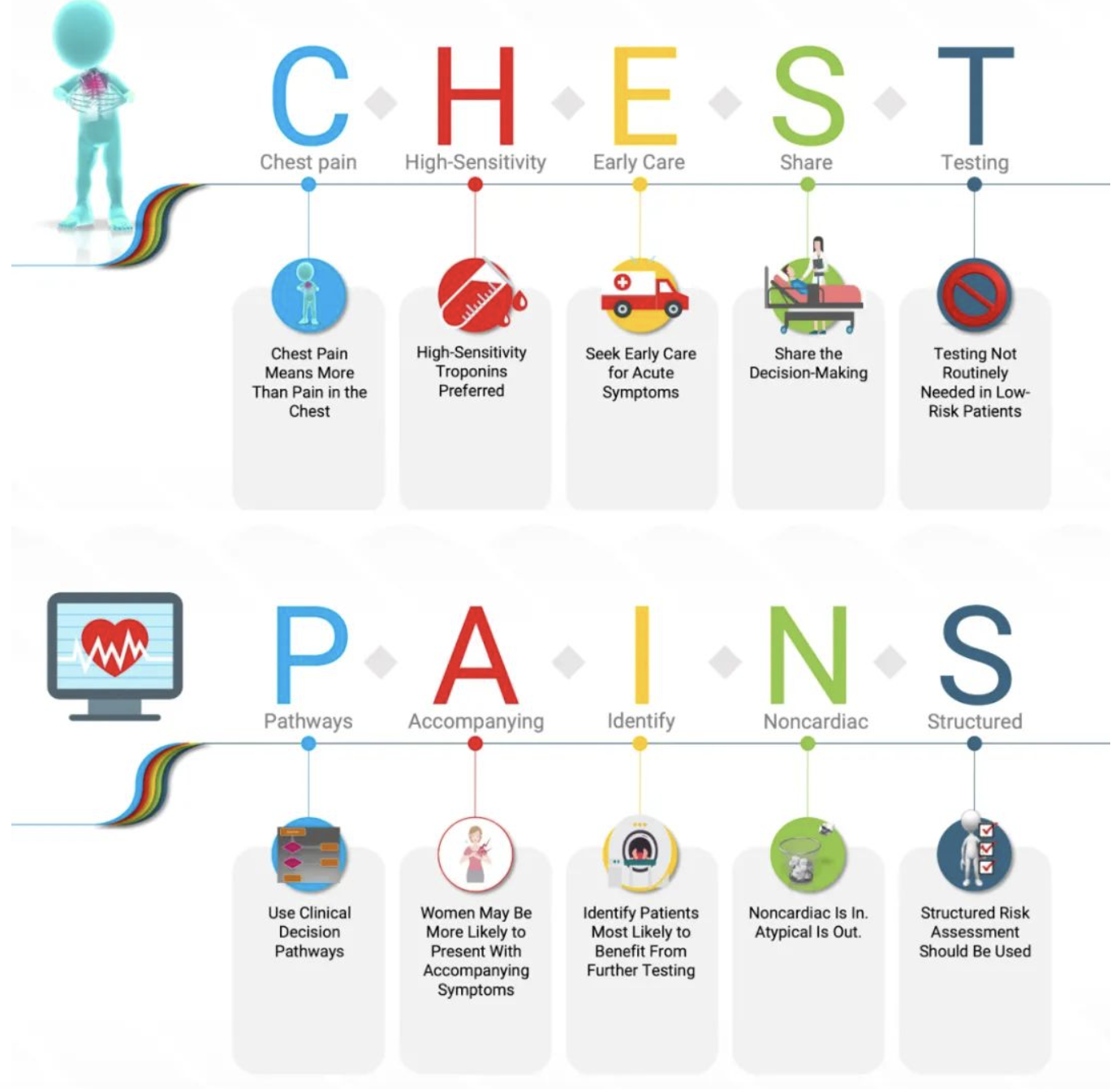
最后,沈节艳教授表示,2021 ACC/AHA胸痛评估与诊断指南对胸痛的标准化风险评估、临床决策路径和诊断工具提出了推荐意见,该指南巧妙的用“CHEST PAINS”表达胸痛的十大重要信息。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#二聚体#
49
#D-二聚体#
48
#OCC#
42
#值班#
49
学习了,
0