Nat Commun:借助博弈论方法揭示临床信息差异化与抗生素滥用的关系
2021-02-20 haibei MedSci原创
研究人员设计了一个模型,在这个模型中,医生在考虑到抗生素的使用会消耗其未来有效性的情况下,权衡是否应该开出抗生素。
对抗生素的耐药性在全球范围内有重大的公共卫生影响。抗生素耐药性感染会增加死亡率,延长住院时间,增加治疗费用。当患者被怀疑有细菌感染时,通常会收集生物标本,进行培养,并进行抗菌素敏感性的测试。一般情况下,几天内就可以知道结果。有了结果,医生就可以开出合适的治疗方案。然而,这些天对于治疗可能是关键的,因此,在确定致病菌之前,医生会给予初步的经验性抗生素治疗。经验性治疗的选择可以基于医生对不同类型感染可能性的非正式评估,基于患者的医疗症状,临床环境和即时诊断测试的结果,或决策支持系统的输出。

抗生素滥用导致耐药的问题是一个典型的公益性难题,适合进行博弈论分析。因此,研究人员设计了一个模型,在这个模型中,医生在考虑到抗生素的使用会消耗其未来有效性的情况下,权衡是否应该开出抗生素。医生的决定依赖于在明确的实验室结果出来之前细菌感染的概率。
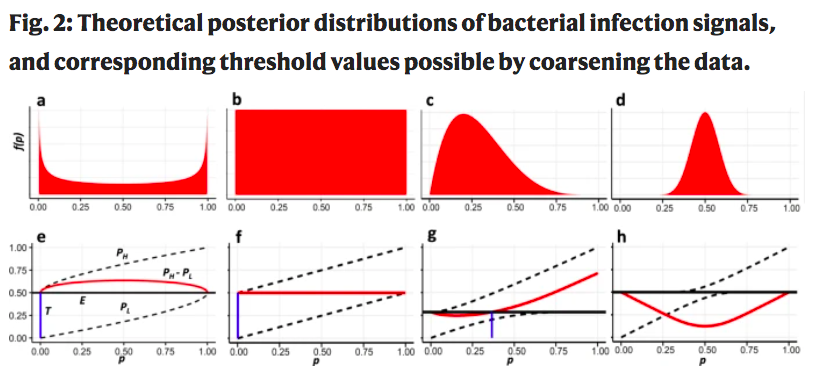
研究人员表明,医生对抗生素处方的均衡决策规则不是社会最优的。研究人员进一步证明,将提供给医生的信息进行离散化处理可以缓解他们的均衡决策与抗生素处方的社会最优之间的差距。尽管这个问题很复杂,但离散化的有效性完全取决于医生可用来确定感染性质的信息类型。
这在理论分布和临床数据集上得到了证明。
因此,该研究结果为当前和未来的抗生素处方决策支持系统的最佳输出提供了一个基于博弈论的指导。
原始出处:
Maya Diamant et al. A game theoretic approach reveals that discretizing clinical information can reduce antibiotic misuse. Nature Communications (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#滥用#
28
#抗生素滥用#
31
#Nat#
29
#COMMUN#
26
好文章!
62