Radiology:人工智能,为低剂量CT筛查肺结节“加装备”!
2021-11-03 shaosai MedSci原创
国家肺部筛查试验(NLST)和荷兰-比利时肺癌筛查试验显示,应用低剂量胸部CT对高危人群进行肺癌筛查可使肺癌死亡率降低20%-26%。

国家肺部筛查试验(NLST)和荷兰-比利时肺癌筛查试验显示,应用低剂量胸部CT对高危人群进行肺癌筛查可使肺癌死亡率降低20%-26%。肺癌在CT上通常表现为肺部结节。然而大多数结节是良性的,并不需要进一步的临床检查。现阶段,临床上已开发出了肺结节管理指南和数据驱动模型,用以减少假阳性的发现率,并进一步避免过度治疗,但要准确区分良性和恶性结节仍然是一个挑战。
近几年,使用卷积神经网络(CNN)的深度学习(DL)算法已成为分析医学图像的首选手段。一些研究通过使用公开的肺部图像数据库联盟的图像收集数据集,展示了CNN在预测肺部结节恶性风险方面的潜力。然而,这些研究使用了放射科医生提供的主观标签,并且缺乏一个客观且坚实的参考标准。
近日,发表在Radiology杂志的一项研究在CNN的基础上开发了一个用于对低剂量CT检测到的肺部结节进行恶性风险评估的DL算法,参考标准由组织病理学检查或至少2年的随访进行设定,并进行了外部验证,为临床肺癌的快速准确筛查及肺结节的良恶性判读提供了技术支持。
本项回顾性研究建立的DL算法是基于2002年至2004年间从国家肺部筛查试验中收集的16 077个结节(1249个恶性)中开发的。在2004年至2010年期间从丹麦肺癌筛查试验中收集的以下三个队列中进行了外部验证:一个包含所有883个结节(65个恶性)的完整队列和两个具有尺寸匹配(175个结节,59个恶性)和没有尺寸匹配(177个结节,59个恶性)的随机选择的良性结节的癌症富集队列。通过使用受试者工作特征曲线下的面积(AUC)来衡量算法的性能,并在全部队列中与Pan-Canadian 肺癌早期检测(PanCan)模型进行比较,在癌症富集队列中与由4名胸腔放射科医生、5名放射科住院医生和2名胸部专业医生组成的11名临床医生进行比较。
在全部队列中,DL算法的表现明显优于PanCan模型(AUC,0.93 [95% CI: 0.89, 0.96] vs 0.90 [95% CI: 0.86, 0.93];P = .046)。在癌症富集队列的随机良性结节(AUC,0.96 [95% CI: 0.93, 0.99] vs 0.90 [95% CI: 0.81, 0.98]; P = .11)和大小匹配的良性结节(AUC,0.86 [95% CI: 0.80, 0.91] vs 0.82 [95% CI: 0.74, 0.89]; P = .26)中,该算法的表现与胸部放射科医生相当。
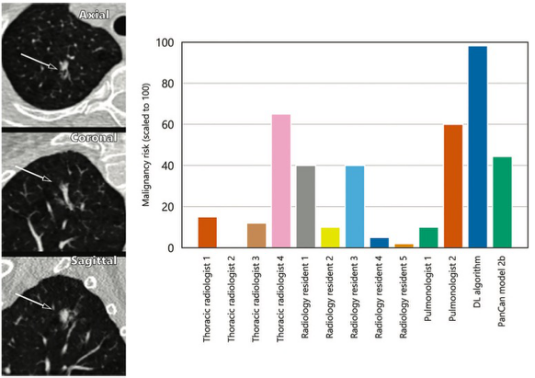
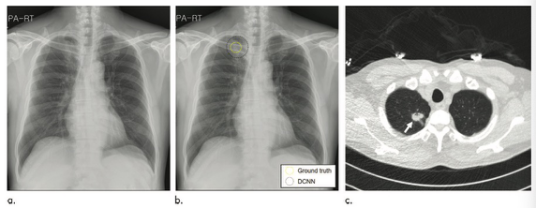
图 丹麦肺癌筛查试验(DLCST)中的一个15毫米的部分实性恶性结节示例。该结节位于右上叶,条形图(右侧)显示,除了一位胸部放射科医生和一位肺科医生外,大多数临床医生都不认为该结节是恶性的。深度学习(DL)算法将这个结节正确地分类为恶性。
本研究成功地开发了一种深度学习算法,该算法可用于对低剂量CT检测到的肺部结节进行恶性肿瘤风险估计,且该算法在不同的筛查人群和方案中具有普遍性。该算法的判别性能可与临床专家相媲美。这种深度学习算法可以协助放射科医生对进行肺癌筛查的参与者进行准确的影像学判读,并可进一步减少不必要的手术。此外,该算法也有助于降低放射科医生的工作量,并减少肺癌筛查的成本。
原文出处:
Kiran Vaidhya Venkadesh,Arnaud A A Setio,Anton Schreuder.Deep Learning for Malignancy Risk Estimation of Pulmonary Nodules Detected at Low-Dose Screening CT.DOI:10.1148/radiol.2021204433
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CT筛查#
64
#低剂量CT#
44
#低剂量#
62
好的
74
学习一下
96