如何看X线片上的肋骨骨折?
2022-07-30 医学影像服务中心 医学影像服务中心
只要是骨头就都有可能会骨折,肋骨也不见得例外。但是肋骨骨折和手足四肢骨骼的骨折有些不同,这是由两方面的因素造成的,一是肋骨的数量,二是肋骨的功能。
只要是骨头就都有可能会骨折,肋骨也不见得例外。但是肋骨骨折和手足四肢骨骼的骨折有些不同,这是由两方面的因素造成的,一是肋骨的数量,二是肋骨的功能。
大多数情况下,正常人一共有十二对肋骨(为什么要这么说?请看《X线片上的肋骨(数量之争)》),在肋骨之间还有肋间肌肉的连结,二者协同合作,构成了人体的胸廓,参与人体的呼吸运动。当人吸气的时候,肋骨前端上抬,胸廓容积变大,气体进入胸腔;当人呼气的时候,肋骨前端下降,胸廓容积缩小,气体则吐出胸外。因为肋骨数量众多,而且相邻肋骨之间又由肌肉连结构成整体,所以单根肋骨的骨折除了会引起疼痛,一般不会在功能上引起大的损害,也不像四肢骨折一般容易发生大的移位。
第一幅:右侧第4肋骨骨折,左侧第5肋骨陈旧性骨折。
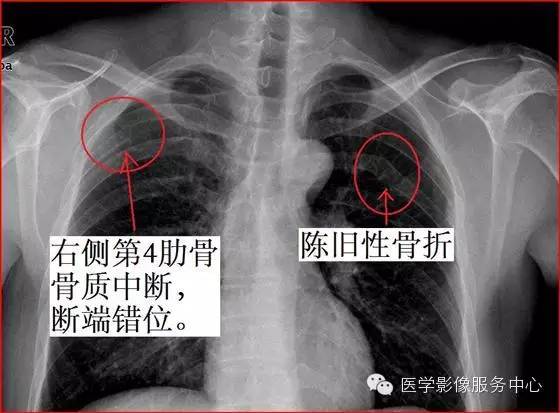
因为单一的肋骨骨折一般不会引起严重的并发症,所以很多时候临床医生并不会针对骨折进行复位内固定等处理,这样靠着肋骨自己慢慢长,等长好以后总会留下一些蛛丝马迹,比如说肋骨变得弯弯曲曲了,或者是肋骨边缘不光整了。
比如下面这幅:左侧第5肋骨陈旧性骨折。

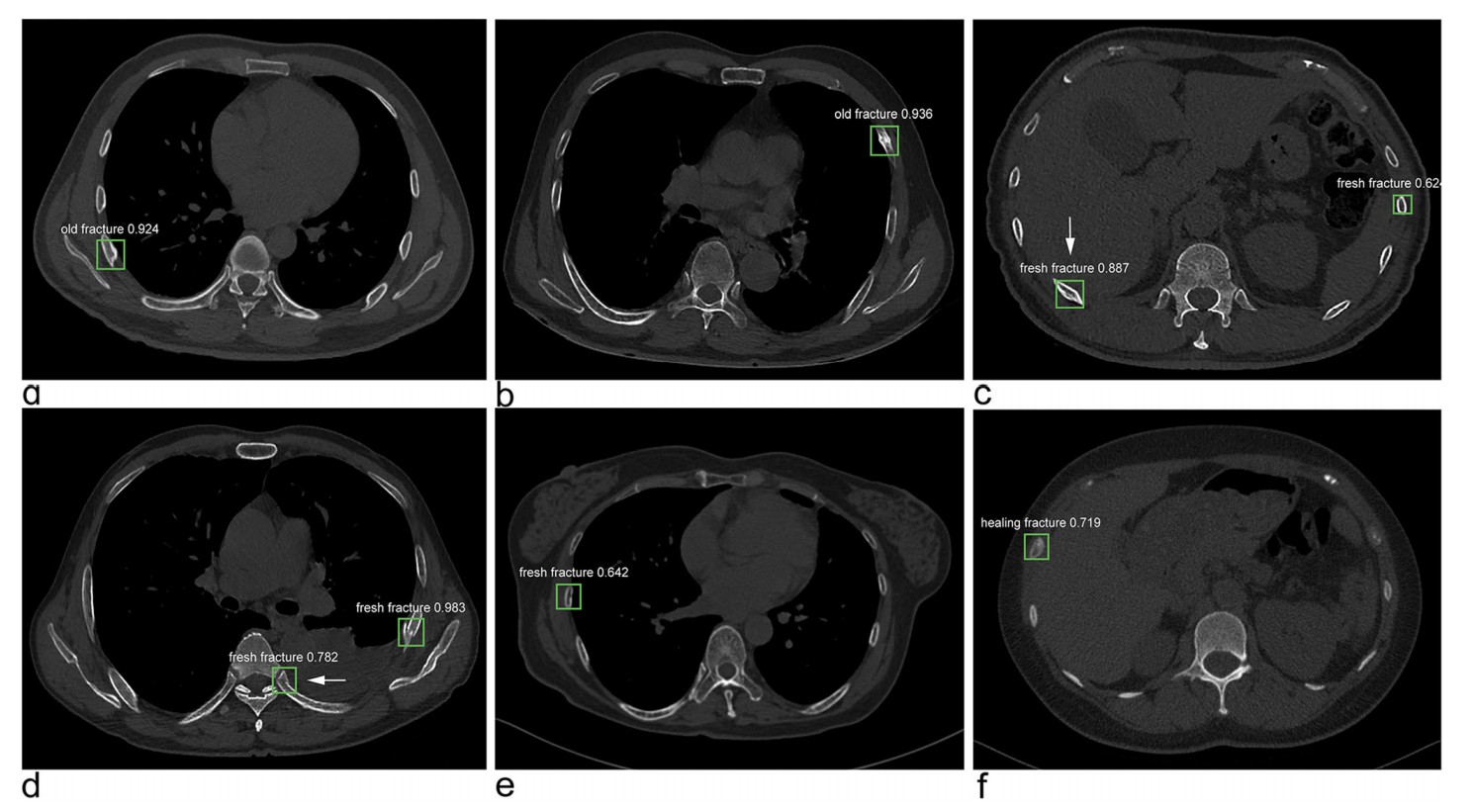
一根肋骨骨折问题不大,两根肋骨骨折一般来说问题也不大:

三根肋骨呢:或许也没事。

……四根呢?五根呢?……
只能说Maybe没事吧,因为如果断的肋骨太多了,就有可能引起“连枷胸”——严重的闭合性胸部损伤导致多根多处肋骨骨折,使局部胸壁失去肋骨支撑而软化,并出现反常呼吸即吸气时软化区胸壁内陷,呼气时外突称为连枷胸。连枷胸常合并有肺挫伤,而且又是诱发急性呼吸窘迫综合征(ARDS)的重要因素。
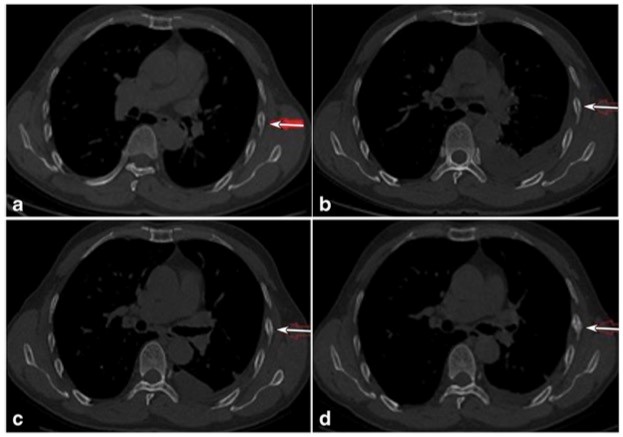
右侧多发肋骨骨折:

左侧多发肋骨骨折:

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#X线#
39
#X线片#
28
#肋骨骨折#
36
学习了
56
学习一下
51