Pain:肝癌患者术后阿片类药物使用与长期手术结局并无相关性
2022-09-12 MedSci原创 MedSci原创
术后阿片类药物不影响因肝细胞癌而接受肝切除术或肝移植患者的总体和无复发生存。癌症复发不应成为术后开出阿片类药物处方的临床顾虑。
肝细胞癌是一种全球性的致命癌症,手术切除仍然是肝细胞癌的标准治疗方法。术后阿片类药物处方被认为通过复杂的生物学途径影响癌症复发。

近日,麻醉疼痛领域权威杂志Pain上发表了一篇研究文章,研究人员采用台湾纵向健康保险数据库进行回顾性队列研究,评估了肝细胞癌患者术后阿片类药物使用与长期手术结局之间的关系。

该研究采用了回顾性队列研究设计,812例年龄大于20岁的患者因肝细胞癌接受了肝脏切除术。暴露组包括术后住院期间使用阿片类药物的患者。对照组包括术后住院期间从未服用过阿片类药物的患者。研究人员采用Cox比例风险模型评估了阿片类药物组与非阿片类药物组的总体生存率或无复发生存率。
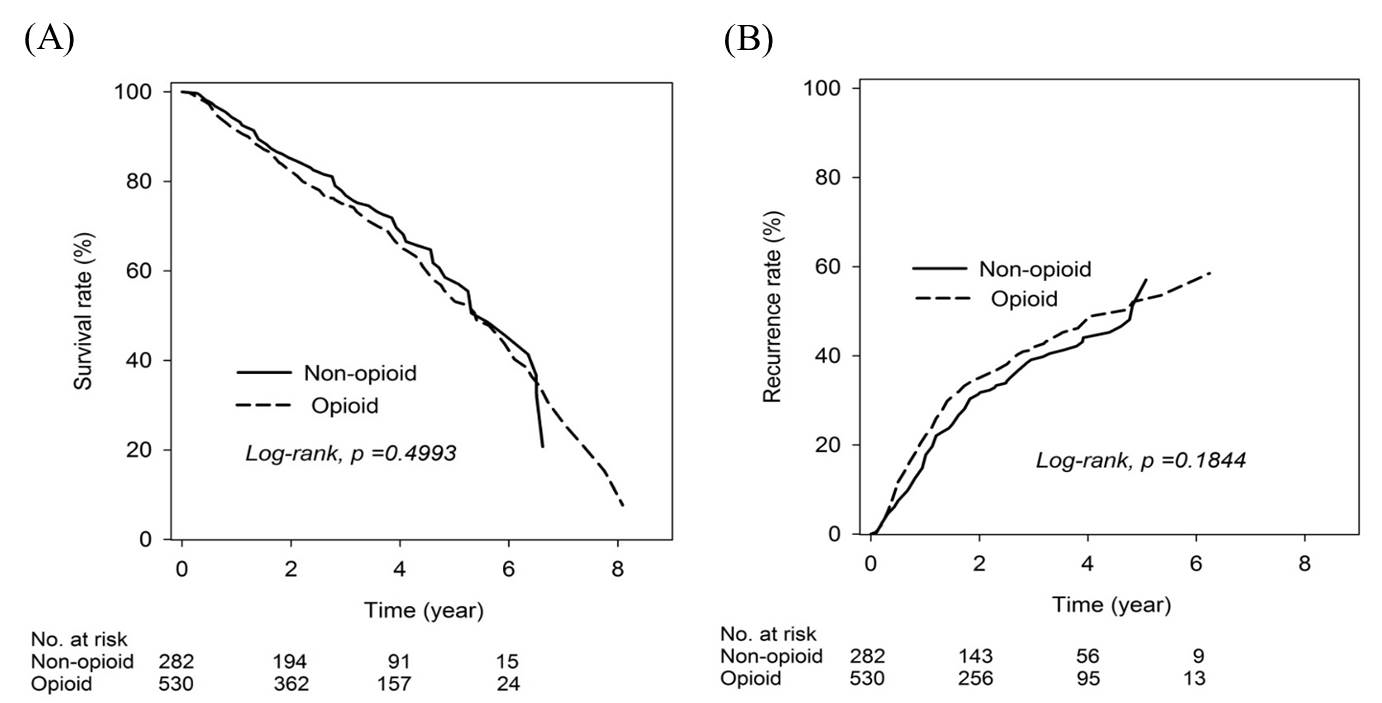
530例患者术后接受阿片类药物治疗,282例患者未接受阿片类药物治疗。总生存期和无复发生存期的风险比分别为1.10(95%CI为0.85-1.41)和1.15(95%CI为0.91-1.46)。术后总阿片类药物转化为口服吗啡毫克当量,然后分成三个相等的亚组:低剂量为<40 mg;中剂量为40 ~ 144 mg;高剂量≥145 mg。低剂量组总生存期的风险比为0.88(95%CI为0.63-1.24),中剂量组风险比为1.27(95%CI为0.92-1.74),高剂量组风险比为1.14(95%CI为0.83-1.58)。
由此可见,术后阿片类药物不影响因肝细胞癌而接受肝切除术或肝移植患者的总体和无复发生存。癌症复发不应成为术后开出阿片类药物处方的临床顾虑。
原始出处:
Yeh, Pin-Hung. et al.No association of postoperative opioid usage with long-term surgery outcomes in patients with liver cancer: a population-based retrospective cohort study.Pain.2022.https://journals.lww.com/pain/Abstract/9900/No_association_of_postoperative_opioid_usage_with.171.aspx
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肝癌患者#
49
#药物使用#
51
#相关性#
44
#阿片类药物#
58
#阿片类#
42