Journal of Cardiovascular Magnetic Resonance:冠脉狭窄是否严重,查一下CMRA
2021-05-18 MedSci原创 MedSci原创
CMRA可对MACE和心源性死亡进行非侵入性危险分层,并且在没有心肌梗塞病史或先前没有冠状动脉血运重建的患者中,提供比常规危险因素更高的预后价值。经CMRA检测的阻塞性CAD及其严重程度与较差预后有关
冠状动脉疾病(CAD)是全球发病率和死亡率的主要原因。早期诊断这种病理有助于指导临床治疗。目前,有创冠状动脉造影被认为是检测CAD的金标准,但其成本较高,且存在并发症风险。冠状动脉CT血管造影(CCTA)已广泛应用于冠状动脉粥样硬化的无创评估。尽管CCTA在评估冠状动脉形态和对未来心脏事件的风险分层方面具有实用价值,但其辐射较大。冠状动脉磁共振血管造影(CMRA)作为一种非侵入性、非电离的冠脉管腔显像方法已经发展了25年,在诊断冠状动脉狭窄方面显示出稳定的改善和有希望的结果。然而,接受CMRA的患者的临床结果数据有限。尽管Yoon等人在随访(中位时间25个月)期间证明了全心CMRA对风险分层的效用,但CMRA的长期预后价值仍不清楚。
Satoshi Nakamura等近期在Journal of Cardiovascular Magnetic Resonance杂志发表文章,其研究目的是评估CMRA的长期预后价值。
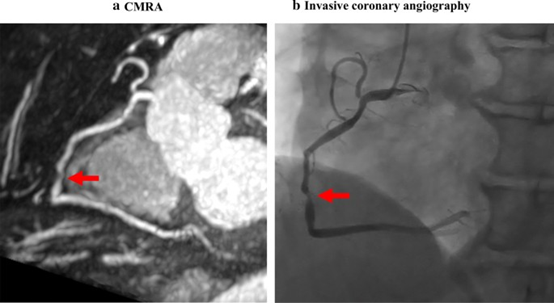
一例66岁女性,有多种危险因素。图示:最大强度投影图像和冠状动脉造影显示右冠状动脉中段明显狭窄(红箭头)
2009年至2015年之间,共有506例无心肌梗塞病史/冠状动脉血运重建史的患者接受了自由呼吸的全心CMRA。使用1.5 T或3 T扫描仪获取图像,并根据两名观察者的一致判断进行视觉评估。CMRA上,阻塞性CAD被定义为至少一支冠状动脉的管腔狭窄≥50%。重大不良心脏事件(MACE)包括心脏死亡,非致命性心肌梗塞,和不稳定的心绞痛。
基于CMRA,214例患者(42%)为阻塞性CAD。在随访期间(中位数为5.6年),发生了31例MACE。Kaplan-Meier曲线分析显示,有阻塞性CAD和无阻塞性CAD的MACE患者的无事件生存率(log-rank, p = 0.003)和心源性死亡(p = 0.012)存在显著差异。无阻塞性CAD、1-血管疾病、2-血管疾病和左主干或3-血管疾病的MACE年发生率分别为0.6%、1.5%、2.3%和3.6%(log-rank,p=0.003)。
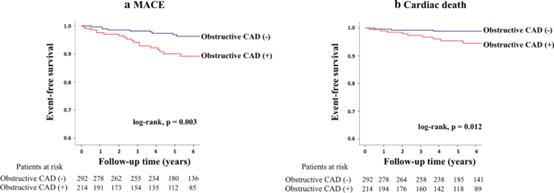
CMRA的长期风险分层。这些数据显示了MACE和心源性死亡的CMRA分级患者无事件生存曲线。

根据CAD严重程度进行风险分层。这些数据显示了MACE CMRA中根据CAD严重程度分层的患者无事件生存曲线,以及根据CAD严重程度的年事件率。

根据1.5 T或3 T扫描仪进行无事件生存分析。该图显示了在进行了场强1.5 T或3 T扫描仪CMR扫描的患者中有无阻塞性CAD的无事件生存曲线。

CMRA相对于临床危险因素的增量值。图中显示的全局卡方检验显示CMRA相对于临床危险因素(年龄、性别、高血压、血脂异常、糖尿病、吸烟和CAD家族史)的预后价值增加。
Cox比例风险回归分析表明,在阻塞性CAD和临床危险因素(年龄,性别,高血压,糖尿病,血脂异常,吸烟和CAD家族史)中,阻塞性CAD和糖尿病是MACE的重要预测指标(HR分别为 2.9 [p = 0.005]和2.2 [p = 0.034])。在多变量分析中,对糖尿病进行调整后,阻塞性CAD仍是一个独立的预测因素(校正后的HR为2.6 [p = 0.010])。将阻塞性CAD添加到临床危险因素中,可将卡方检验结果从8.3显着提高到13.8(p = 0.022)。
这是第一个评估全心CMRA长期预后价值的研究。在中位5.6年的随访期间,CMRA显示冠状动脉管腔狭窄是MACE的独立预测因素。CMRA无阻塞性CAD的患者未来发生心脏事件的风险较低。全心自由呼吸CMRA可对MACE和心源性死亡进行非侵入性危险分层,并且在没有心肌梗塞病史或先前没有冠状动脉血运重建的患者中,提供比常规危险因素更高的预后价值。经CMRA检测的阻塞性CAD及其严重程度与较差预后有关。重要的是,CMRA无阻塞性CAD的患者预后良好。
综上所述,自由呼吸全心CMRA允许患者在无辐射的情况下,通过冠脉可视化进行长期风险分层。CMRA检测到的阻塞性CAD的存在和严重程度与较差的预后相关。更重要的是,CMRA上无阻塞性CAD患者的事件发生率为1%,这与CCTA对预后价值的研究结果一致。此外,与传统的危险因素相比,目前的研究结果显示了额外的预后价值。无创成像在风险分层中的价值一直是一个热门话题,关于是否应该将无创成像纳入常规风险分层工具和指南的争论。该研究通过提出一种结合CMRA和常规风险因素的风险分层方案,可能为这一争论提供一个新的视角。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#ASC#
0
#Resonance#
44
#CMR#
0
#冠脉狭窄#
39
#vascular#
37
#NET#
29
#ESO#
0
#cardiovascular#
36
#MRA#
36
阻塞性CAD
64