Stroke : 凝血障碍导致的脑出血,andexanet alfa治疗并未改变临床预后
2021-10-18 Freeman MedSci原创
与常规护理相比,andexanet alfa与创伤性因子Xa抑制剂相关ICH的较低HE率有关
长期口服抗凝剂(OAC)最重要的并发症是脑内出血(ICH),它与不良的预后和高院内死亡率有关。自从直接作用口服抗凝剂(DOACs)上市以来,使用维生素K拮抗剂治疗的OAC患者的比例正在下降,DOACs正在被优先使用,部分原因是与维生素K拮抗剂相比,ICH发生的风险减半。

然而,直到最近,在发生大出血时,DOACs缺乏抗凝逆转的特异性解毒剂,而凝血酶原复合物浓缩物(PCCs)作为华法林的特异性解毒剂被广泛使用。
Idarucizumab和andexanet alfa代表了DOAC相关出血的止血治疗的特异性解毒剂,并在以前的试验中显示了有希望的结果。来自达比加群相关中风的真实世界数据表明,除了出色的止血效果外,idarucizumab还有临床益处。
虽然已经公布了服用因子Xa抑制剂(fXi)的DOAC患者在大出血中使用PCC的真实世界数据,但仍需要使用andexanet alfa治疗与服用fXi-intake(fXi-ICH)有关的ICH患者的止血效果和临床结果的真实世界数据。
鉴于关于PCC治疗fXi-ICH的止血效果的报告相互矛盾,对andexanet alfa与PCC在放射学和临床结果方面进行头对头的比较将是有价值的。虽然正在进行的ANNEXA-I试验(Andexanet Alfa,一种新的因子Xa抑制剂抗凝作用的解毒剂)在随机前瞻性研究设计中解决了这个问题,但最近发表的病例系列和未经调整的注册数据提供了有限的比较数据,而且比较没有调整混杂因素,如基线血肿体积。
藉此,德国University Hospital Erlangen的Hagen B. Huttner等人,探讨了与包括PCC在内的常规护理相比,使用andexanet alfa治疗是否与血肿扩大(HE)率的降低和创伤性fXi-ICH患者临床结果的改善有关。
研究数据提取自多中心、前瞻性、单臂ANNEXA-4试验(Andexanet Alfa,一种新的因子Xa抑制剂抗凝作用的解毒剂)和多中心观察性队列研究RETRACE-II(German-Wide Multicenter Analysis of Oral Anticoagulant-Associated Intracerebral Hemorrhage - Part Two)。
脑出血是基于基线成像后36小时内进行的计算机断层扫描。为调整基线合并症和ICH的严重程度,进行了逆向治疗概率加权。
入院后18小时内接受阿哌沙班或利伐沙班治疗的非创伤性ICH患者被纳入。患有继发性ICH或不符合ANNEXA-4试验纳入标准的患者被排除。
他们将接受andexanet alfa止血治疗的ANNEXA-4患者与RETRACE-II患者进行了比较,后者接受常规治疗,主要是给予凝血酶原复合物浓缩液。主要结果是HE的比率,定义为相对增加≥35%。次要结果包括血肿体积的平均绝对变化,以及院内死亡率和功能结果。
他们发现:总的来说,182名因子Xa抑制剂相关的ICH患者(85名接受andexanet alfa,97名接受常规护理)被选作分析对象。
两组之间在人口统计学或临床特征方面没有相关差异。80名andexanet alfa患者中有11名(14%)发生了血栓,而67名常规护理患者中有21名(36%)发生了血栓(调整后的相对风险,0.40[95%CI,0.20-0.78];P=0.005),平均整体血肿体积变化减少7毫升。
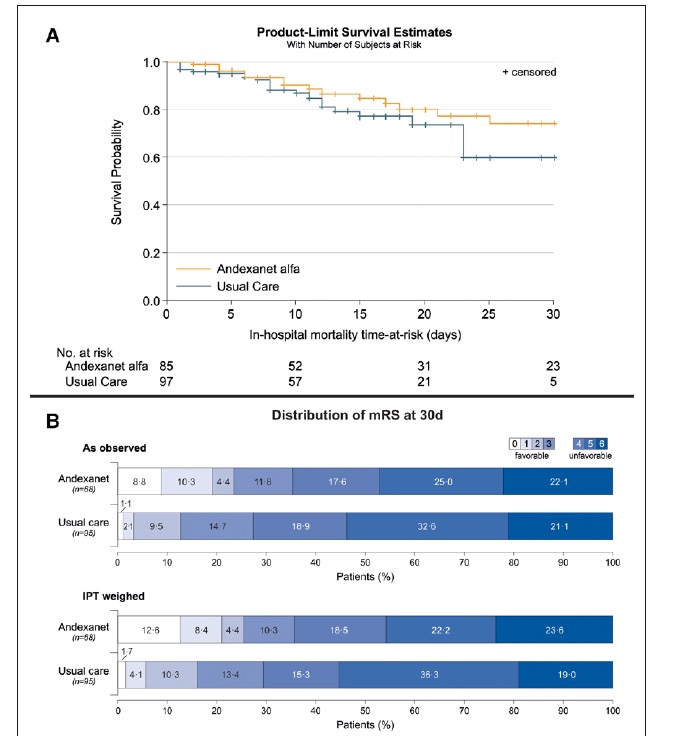
在院内死亡率或功能结果方面没有统计学上的显著差异。敏感性分析仅包括接受凝血酶原复合物浓缩液的常规护理患者,结果一致。
该研究的重要意义在于发现了:与常规护理相比,andexanet alfa与创伤性因子Xa抑制剂相关ICH的较低HE率有关,然而,没有转化为明显改善的临床结果。需要进行比较试验来证实限制HE的益处,并探讨不同患者亚组和治疗时间的临床结果。
原文出处:
Huttner HB, Gerner ST, Kuramatsu JB, et al. Hematoma Expansion and Clinical Outcomes in Patients With Factor-Xa Inhibitor–Related Atraumatic Intracerebral Hemorrhage Treated Within the ANNEXA-4 Trial Versus Real-World Usual Care. Stroke. Published online October 14, 2021:STROKEAHA.121.034572. doi:10.1161/STROKEAHA.121.034572
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#ALF#
43
#NET#
44
#DEXA#
34
#andexanet#
34
#临床预后#
49
#凝血障碍#
42