Neurology :浙江大学:双侧基底节动脉堵塞,越早治疗效果越好
2021-10-23 Freeman MedSci原创
在常规的急性基底动脉闭塞患者中,在发病后的头9小时内,较早的EVT治疗与较好的预后有关,但之后的获益可能维持不变。
基底动脉闭塞(BAO)在没有再通的情况下有很高的发病率和死亡率1。越来越多来自多中心的前瞻性或回顾性队列的证据表明,血管内治疗(EVT)对BAO患者有益。尽管最近的BEST(基底动脉闭塞血管内介入治疗与标准药物治疗的比较)试验由于交叉率高和招募不力,在意向性治疗分析中未能支持EVT优于药物治疗,但实际上在8小时内接受EVT治疗的BAO患者比接受标准药物治疗的患者取得了更好的结果(47% vs 24%)。
发病到穿刺时间(OPT)被认为是提供EVT的一个实用和有用的临床标志。来自急性前部大血管闭塞的证据表明,较早进行EVT会有较强的时间依赖性。
然而,目前调查OPT与BAO患者结果之间关系的数据是有限的和不一致的。一些研究表明,OPT与急性BAO的预后没有关系,而其他研究表明,治疗时间对急性BAO患者至关重要。
由于样本量不大,这些统计力度(statistical power)不足,对当前临床实践的普遍性也不确定。2019年,美国心脏协会/美国卒中协会指南指出,在卒中发病6小时内启动血栓切除术,对精心挑选的BAO患者可能是合理的(IIb类,证据等级C)。
然而,在日常实践中,干预者一般采用较长的时间窗口对急性BAO进行EVT,尽管这还没有完全确定。为了指导急性BAO中EVT的进一步改进,需要更多关于OPT与预后之间关系的证据。
藉此,浙江大学的Hongfei Sang等人,利用急性基底动脉闭塞的血管内治疗研究(BASILAR)的数据,旨在评估OPT如何影响目前临床实践中急性BAO患者的EVT的疗效和安全结果。并研究EVT的受益程度随着治疗时间的延迟而改变。
他们利用急性基底动脉闭塞的EVT(BASILAR)研究,确定了2014年1月至2019年5月在中国47家综合卒中中心接受EVT的急性基底动脉闭塞的连续患者。主要结果是90天后的良好功能结果(定义为修改的Rankin量表评分[mRS]0-3)。次要结果包括功能独立(mRS 0-2)、死亡率和症状性脑内出血。使用多变量逻辑回归(OPT为分类变量)和限制性立方样条回归(Restricted cubic spline regression analysis )(OPT为连续变量)分析OPT与临床结果的关系。
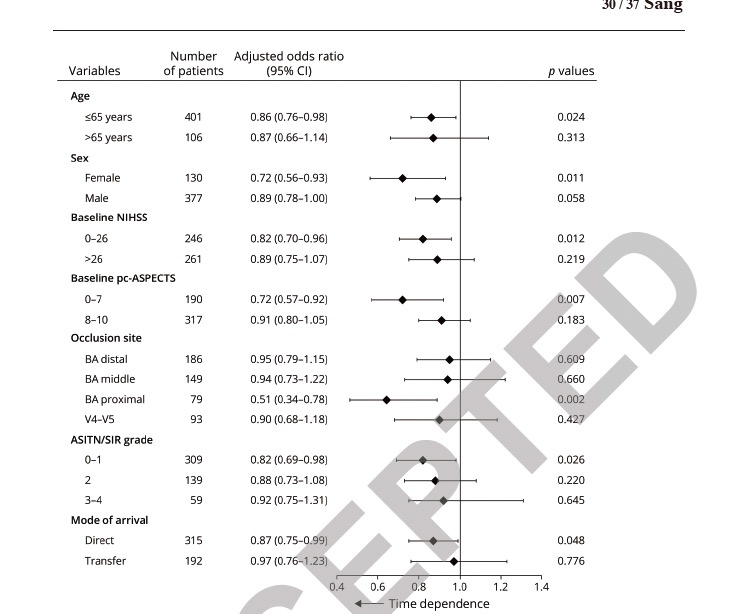
他们发现:在639名符合条件的患者中,年龄中位数为65岁,OPT中位数为328分钟(四分位数范围,220-490)。与4-8小时内的治疗相比,4-8小时和8-12小时内的治疗与较低的有利结果率有关(调整后的OR值分别为0.63 [95% CI, 0.40-0.98]和0.47 [95% CI, 0.23-0.93])。
限制性立方样条回归分析显示,OPT与有利的结果(P非线性=0.028)和功能独立(P非线性=0.025)有L型关联,在整个前9小时有明显的利益损失,但随后出现相对平缓。
OPT的死亡率在9小时内相对增加,但随后趋于平缓(P非线性=0.042)。症状性脑内出血与OPT之间的关联并不显著。
这个研究的重要意义在于发现了:在常规的急性基底动脉闭塞患者中,在发病后的头9小时内,较早的EVT治疗与较好的预后有关,但之后的获益可能维持不变。
原文出处:
Sang H fei, Yuan J jie, Qiu Z, et al. Association Between Time to Endovascular Therapy and Outcomes in Patients With Acute Basilar Artery Occlusion. Neurology. Published online October 14, 2021:10.1212/WNL.0000000000012858. doi:10.1212/WNL.0000000000012858
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#Neurol#
39
#浙江大学#
57
#治疗效果#
40
#早治疗#
40
#双侧#
35
#基底节#
37