JAMA Oncology:三阴性乳腺癌新辅助化疗后ctDNA与CTCs阳性患者预后更差
2020-07-17 Muse Fan MedSci原创
目前,三阴性乳腺癌患者中有很大一部分接受新辅助化疗,其中,三分之二的患者会有病灶残留,并且有很高的复发风险。
三阴性乳腺癌(Triple-negative breast cancer, TNBC)是指乳腺癌患者雌激素受体(ER)、孕激素受体(PR)和原癌基因HER-2均为阴性,是乳腺癌病理分型中预后最差的一个类型。目前,TNBC患者中有很大一部分接受新辅助化疗,大约三分之一的患者通过新辅助化疗能够获得比较好的临床治疗效果,而三分之二的患者会有病灶残留,并且有很高的复发风险。术后通过检测循环血液中微小残留病(minimal residual disease,MRD)的方法可以用来判断患者是否会出现疾病的复发。基于液体活检的循环肿瘤DNA(ctDNA)和循环肿瘤细胞(CTCs)分析是检测MRD的常用方法。那么对于早期TNBC患者,术后ctDNA和CTCs的检测是否可以判断疾病预后呢?
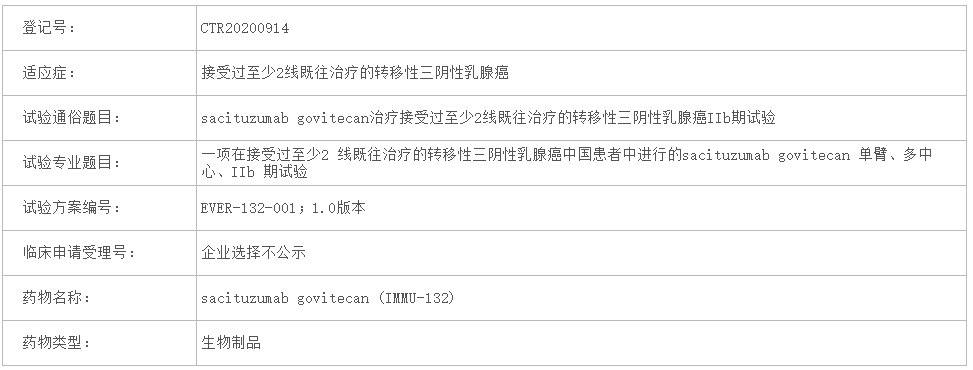
近日,发表在《JAMA Oncology》的一篇论文对一项196名女性患者的临床研究进行了二次分析,分析了其中142名患者ctDNA与生存期的相关性及123名患者CTCs与生存期的相关性。
结果显示:ctDNA阳性患者的无远处转移生存期DDFS、无病生存期DFS和总生存期OS都显著低于ctDNA阴性患者,风险比HR分别为2.99,2.67和4.16;而ctDNA与CTCs的结合检测对于判断预后有着更高的灵敏性和特异性,与ctDNA和CTCs均为阴性患者相比,两者均为阳性的患者无远处转移生存期DDFS、无病生存期DFS和总生存期OS均明显低于阴性患者,风险比HR分别为5.29,3.15和8.60。
研究得出:ctDNA和CTCs的检测对于临床试验中的患者风险分层具有指导意义。为寻求更精准和个体化的治疗效果,该研究计划在后续实验中对ctDNA阳性患者进行基于血浆测序结果的靶向治疗。
原始出处:
Radovich M, Jiang G, Hancock BA, Chitambar C, Nanda R, Falkson C, et al. Association of Circulating Tumor DNA and Circulating Tumor Cells After Neoadjuvant Chemotherapy With Disease Recurrence in Patients With Triple-Negative Breast Cancer: Preplanned Secondary Analysis of the BRE12-158 Randomized Clinical Trial. JAMA Oncol 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
32
#TCS#
40
#CTCs#
35
#新辅助#
29
#阴性乳腺癌#
32
#CTC#
41
#Oncology#
38
#患者预后#
29
#三阴性#
24
阐述清晰明了
82