Ann Surg:术中输血怎么输?真的有标准的输血指征和方案吗?
2021-06-13 MedSci原创 MedSci原创
现有的指南在其建议中存在很大差异,并且缺乏足够的术中证据基础。这代表了文献中一个主要的知识缺口。
红细胞(RBC)输血是世界范围内最常见的医疗干预手段之一。仅在美国,每年就有1100万单位的红细胞被使用,其中超过四分之一的红细胞被用于外科病人。在手术过程中,当有临床指示时,输血可能挽救生命,但有时也可能因管理不当对患者造成伤害。
与输血不足导致的器官末端缺血的直接风险相比,它们的短期风险描述得很清楚,其中,早期风险包括0.1%-8%的患者发生输血相关急性肺损伤,以及3.5%-5%的患者发生输血相关循环超负荷,这已成为输血相关死亡的主要原因。相比之下,由于观察性研究中的指征混淆,长期风险尚未被完全理解,也是在文献中争论的主题。

鉴于输血相关的免疫调节、术后并发症和可能更糟糕的癌症特异性结果的报道,手术中过度输血的风险是外科医生和患者都非常关注的问题。最后,考虑到血液的成本和有限的供应,外科过度输血也是卫生保健管理人员关注的问题。
基于这些,有研究小组对有关术中红细胞(RBC)输血的临床实践指南(CPGs)在适应症、决策和支持证据基础方面进行系统的回顾。该研究结果近日发表在了Annals of Surgery期刊上。
研究者系统地检索了电子数据库(MEDLINE、EMBASE和CINAHL)、指南交换所和谷歌Scholar,以查找与术中RBC输血指证有关的临床实践指南(CPG)。检索合格的指南使用AGREE II对其质量进行评估。对相关建议进行了摘要和综合,以便在准则之间进行比较。
研究数据发现,1992年至2018年间公布的10项指南提供了术中输血的适应症。没有指南将术中输血决策作为其主要关注点。六项指南提供了基于血红蛋白(范围6.0-10.0 g/dL)或红细胞压积(<30%)触发因素的输血标准。在缺乏客观输血规则的情况下,CPGs建议考虑其他参数,如失血(n=7)、终末器官缺血(n=5)和血流动力学(n=4)。支持术中输血的建议证据主要是从非手术环境中推断出来的。根据AGREEⅡ评分,纳入指南的质量存在很大差异。
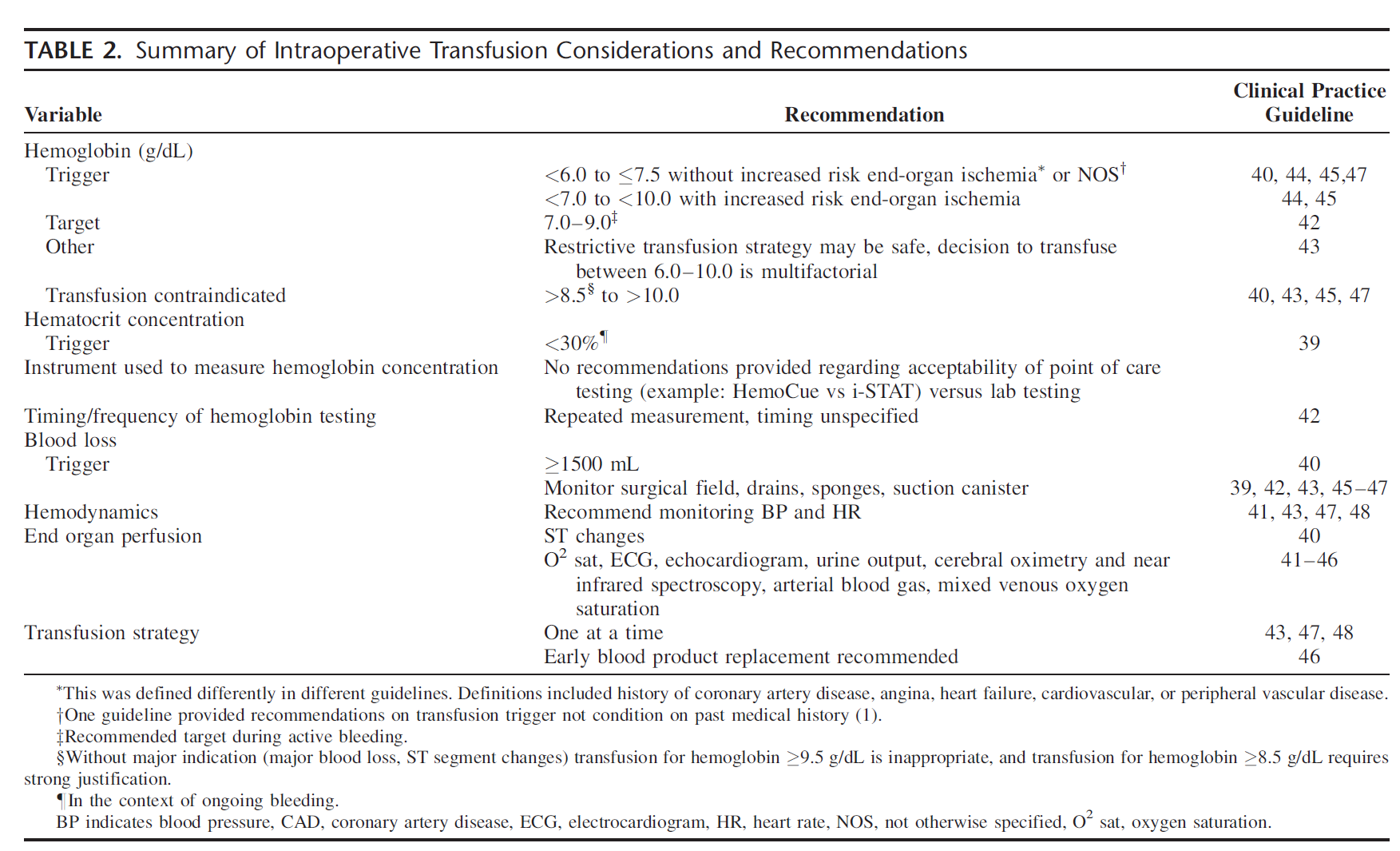
术中输血的考虑和建议
大多数指南(n=7)建议在决定是否在手术室给病人输血时首先考虑失血量。渥太华肝切除术中适当输血的标准规定,严重失血是输血的适应症,在指南正文中量化为1500毫升。另一项指南指出,在大量失血的情况下,在体外循环中输注血红蛋白高于6.0g/dL的患者是合适的。
其余的指南建议监测失血量而不提供输血指征。例如,他们建议临床医生对失血动态进行反复测量或注意失血。美国麻醉师学会围手术期血液管理特别工作组建议对外科领域进行视觉评估,包括血液存在的程度、微血管出血的存在、外科海绵、血栓大小和形状以及吸入罐的容积。
儿科危重病输血和贫血专家倡议的指南建议除了血红蛋白浓度(即症状、体征、生理标志物、实验室结果)外,还要考虑整体的临床情况。
这篇综述确定了几个临床实践指南,为术中输血提供建议。但研究小组注意到,现有的指南在其建议中存在很大差异,并且缺乏足够的术中证据基础。这代表了文献中一个主要的知识缺口。
参考文献:Baker, Laura MD∗,†; Park, Lily MD∗; Gilbert, Richard MD∗; Ahn, Hilalion MD∗; Martel, Andre MD∗; Lenet, Tori MD∗,†; Davis, Alexandra MSc‡; McIsaac, Daniel I. MD, FRCPC†,§; Tinmouth, Alan MD, FRCPC†,¶,||; Fergusson, Dean A. PhD∗,†,¶,||; Martel, Guillaume MD, FRCSC, FACS∗,† Intraoperative Red Blood Cell Transfusion Decision-making, Annals of Surgery: July 2021 - Volume 274 - Issue 1 - p 86-96 doi: 10.1097/SLA.0000000000004710
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#输血#
48
十分有帮助
48
学习了
50
受益
47
学习了
65